Wolff-Parkinson-White Syndrome, commonly abbreviated as WPW, is a rare heart condition that affects the electrical pathways of the heart. This condition causes an abnormal heartbeat, which can lead to various symptoms and complications if left untreated. In this article, we will explore the details of this syndrome, including its causes, symptoms, and available treatments.
What is Wolff-Parkinson-White Syndrome?
Wolff-Parkinson-White Syndrome is a congenital heart condition characterized by an extra electrical pathway in the heart. This additional pathway disrupts the normal rhythm of the heart, causing episodes of rapid heartbeats. The syndrome is named after the three doctors—Louis Wolff, John Parkinson, and Paul Dudley White—who first described it in 1930.
The presence of this extra pathway allows electrical signals to bypass the normal conduction system of the heart. As a result, the heart may beat too quickly, leading to palpitations, dizziness, or even fainting. While some individuals with this condition may never experience symptoms, others may face serious complications, such as arrhythmias or cardiac arrest.
Causes of Wolff-Parkinson-White Syndrome
The exact cause of this syndrome is not fully understood, but researchers believe it is primarily a congenital condition, meaning it is present at birth. Below are some key factors associated with the development of this condition:
- Congenital Heart Abnormalities: Most cases of the syndrome occur due to an abnormality in the development of the heart during fetal growth. The extra electrical pathway forms as the heart develops, leading to the characteristic symptoms of the condition.
- Genetic Factors: Some studies suggest that genetics may play a role in the development of this condition. Individuals with a family history of heart rhythm disorders may have a higher risk of developing this syndrome.
- Idiopathic Cases: In some instances, no clear cause can be identified. These cases are referred to as idiopathic, meaning they arise spontaneously without a known origin.
Symptoms of Wolff-Parkinson-White Syndrome
The symptoms of this condition can vary widely from person to person. Some individuals may remain asymptomatic throughout their lives, while others may experience severe symptoms that require immediate medical attention. Common symptoms include:
- Rapid Heartbeat: One of the hallmark symptoms of this condition is a sudden increase in heart rate, also known as tachycardia. This can occur sporadically and may last for a few seconds to several hours.
- Palpitations: Many individuals describe feeling their heart “flutter” or “race.” These sensations can be alarming and may interfere with daily activities.
- Dizziness or Lightheadedness: Due to the irregular heartbeat, blood flow to the brain may be temporarily reduced, leading to feelings of dizziness or lightheadedness.
- Fainting: In more severe cases, the heart’s inability to pump blood effectively can result in fainting spells, also known as syncope.
- Chest Pain: Some individuals may experience chest discomfort or pain during episodes of rapid heartbeats.
- Shortness of Breath: Difficulty breathing may occur, especially during physical activity or when the heart is beating rapidly.
It is important to note that these symptoms can mimic those of other heart conditions, so proper diagnosis by a healthcare professional is essential.
Diagnosis of Wolff-Parkinson-White Syndrome
Diagnosing this condition typically involves a combination of medical history evaluation, physical examination, and specialized tests. Below are some common diagnostic methods used:
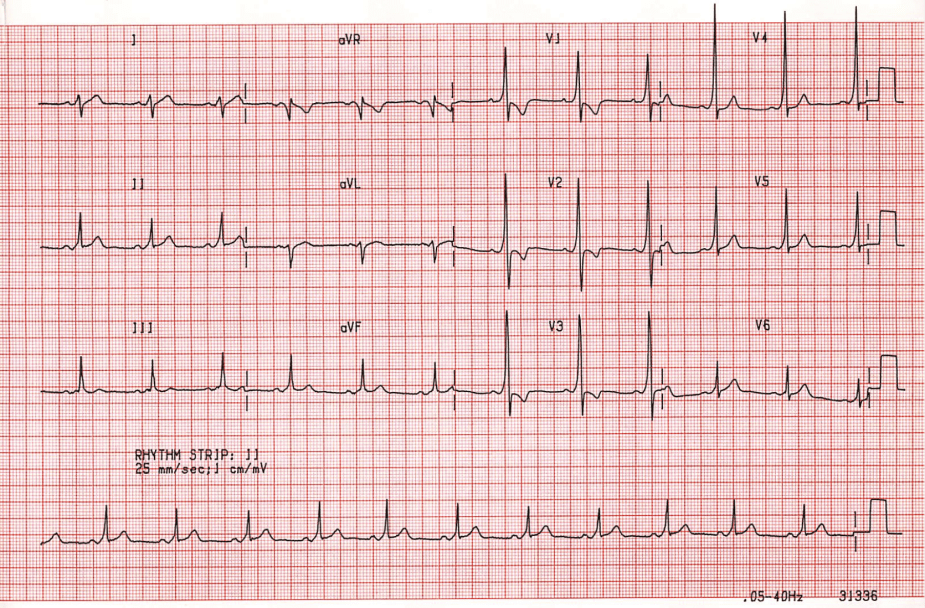
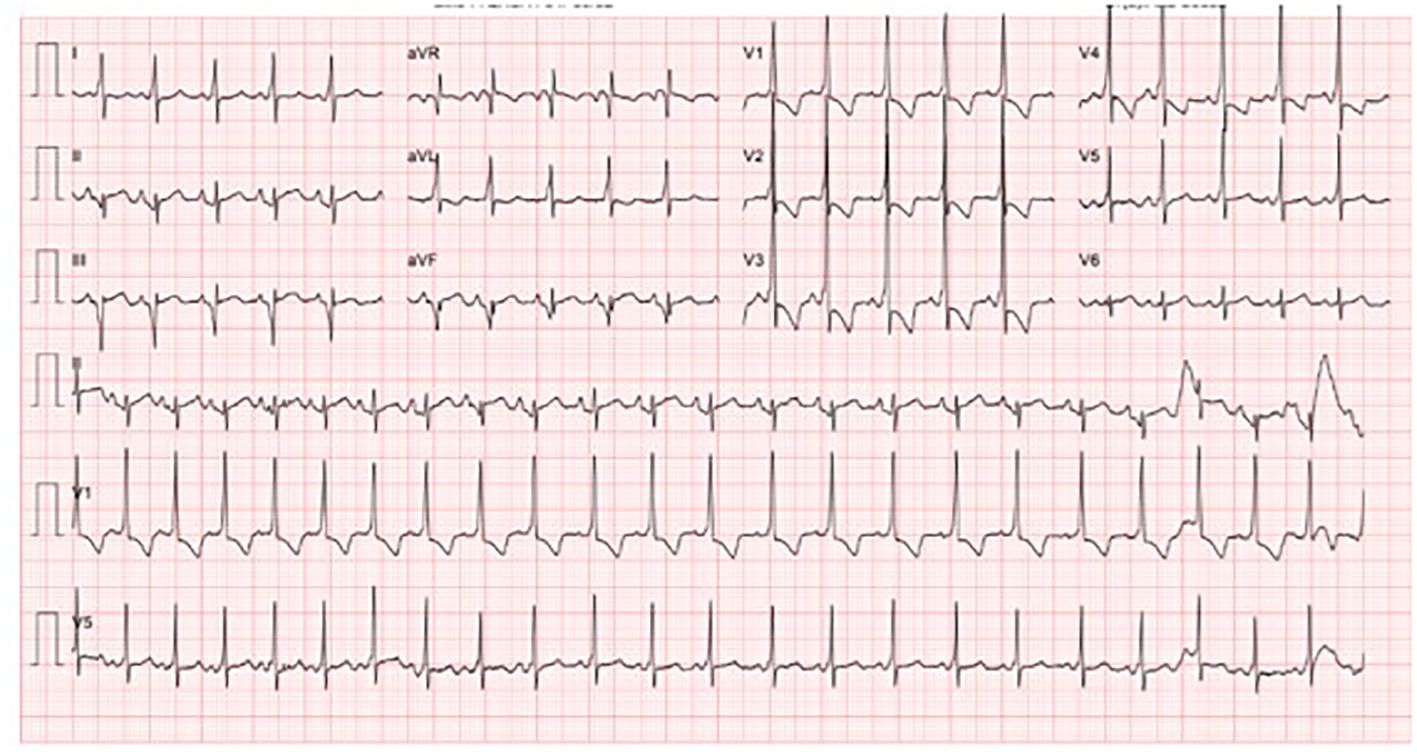
Electrocardiogram (ECG)
An electrocardiogram is one of the primary tools used to diagnose this condition. It records the electrical activity of the heart and can detect the presence of an extra pathway. A distinctive pattern on the ECG, known as a “delta wave,” is often indicative of the syndrome.
Holter Monitor
A Holter monitor is a portable device that records the heart’s activity over a 24- to 48-hour period. This test is particularly useful for capturing intermittent episodes of rapid heartbeats that may not occur during a standard ECG.
Electrophysiology Study
In some cases, a more invasive test called an electrophysiology study may be performed. During this procedure, thin wires are inserted into the heart through a vein to map the electrical activity and identify the location of the extra pathway.
Treatments for Wolff-Parkinson-White Syndrome
The treatment approach for this condition depends on the severity of symptoms and the individual’s overall health. In mild cases, no treatment may be necessary, while more severe cases may require intervention. Below are some common treatment options:
Lifestyle Modifications
For individuals with mild symptoms, lifestyle changes may help manage the condition. These include:
- Avoiding stimulants such as caffeine, nicotine, and alcohol
- Practicing stress-reduction techniques like yoga or meditation
- Maintaining a healthy diet and regular exercise routine
Medications
Several medications can help control the heart’s rhythm and prevent episodes of rapid heartbeats. Commonly prescribed drugs include:
- Antiarrhythmic Medications: These drugs help regulate the heart’s rhythm and prevent abnormal electrical signals.
- Beta-Blockers: These medications slow the heart rate and reduce the workload on the heart.
Catheter Ablation
Catheter ablation is a minimally invasive procedure that has become a popular treatment option for this condition. During the procedure, a catheter is guided to the heart, and radiofrequency energy is used to destroy the extra electrical pathway. This effectively cures the condition in most cases and eliminates the need for long-term medication.
Emergency Treatment
In cases where an individual experiences a life-threatening arrhythmia, emergency treatment may be required. This can include:
- Vagal Maneuvers: Techniques such as bearing down or applying cold water to the face can sometimes slow the heart rate temporarily.
- Cardioversion: A controlled electric shock may be administered to restore the heart’s normal rhythm.
Living with Wolff-Parkinson-White Syndrome
While living with this condition can be challenging, many individuals are able to lead normal, active lives with proper management. Regular follow-up appointments with a cardiologist are essential to monitor the condition and adjust treatment as needed. Additionally, individuals should be aware of warning signs that may indicate a worsening of symptoms, such as prolonged episodes of rapid heartbeats or fainting spells.
Support and Education
Joining support groups or seeking educational resources can be beneficial for individuals and families affected by this condition. Understanding the nature of the syndrome and learning how to manage symptoms can empower patients to take an active role in their healthcare.
Precautions During Physical Activity
Individuals with this condition should consult their healthcare provider before engaging in strenuous physical activities. While moderate exercise is generally safe, certain activities that place excessive strain on the heart may need to be avoided.
Complications Associated with Wolff-Parkinson-White Syndrome
If left untreated, this condition can lead to serious complications, including:
- Atrial Fibrillation: An irregular and often rapid heart rate that can increase the risk of stroke.
- Ventricular Fibrillation: A life-threatening arrhythmia that requires immediate medical intervention.
- Sudden Cardiac Arrest: In rare cases, the condition can lead to a complete loss of heart function.
Early diagnosis and appropriate treatment can significantly reduce the risk of these complications.
Conclusion
Wolff-Parkinson-White Syndrome is a complex heart condition that requires careful management. By understanding its causes, recognizing its symptoms, and exploring available treatments, individuals can take proactive steps to safeguard their heart health. With advancements in medical technology and ongoing research, the outlook for those living with this condition continues to improve.