Vitiligo, often abbreviated as VL, is a chronic skin condition that affects millions of people worldwide. It is characterized by the loss of pigment in patches of skin, leading to uneven skin tone and, in some cases, significant emotional distress. Despite its prevalence, vitiligo remains widely misunderstood, with many people unaware of its causes, symptoms, and available treatments. This article aims to shed light on this complex disorder, exploring its origins, progression, and impact on those who live with it.
What Is Vitiligo?
Vitiligo is a long-term condition where pale or white patches develop on the skin due to the loss of melanin, the pigment responsible for giving skin its color. Melanin is produced by cells called melanocytes, and when these cells stop functioning or die, the result is depigmented areas on the skin. These patches can appear anywhere on the body, including the face, hands, arms, legs, and even inside the mouth or on the scalp.
The condition can affect individuals of all ages, genders, and ethnic backgrounds, though it is more noticeable in people with darker skin tones. The onset of vitiligo can occur at any age, but it most commonly begins before the age of 20.
Symptoms of Vitiligo
- Patchy Loss of Skin Color: The hallmark symptom of vitiligo is the appearance of white or depigmented patches on the skin. These patches may start small but can expand over time.
- Premature Graying: Some individuals with vitiligo experience premature graying of hair on the scalp, eyebrows, eyelashes, or beard.
- Discoloration in Mucous Membranes: The condition can also cause a loss of color in the tissues lining the mouth, nose, or genitals.
- Changes in Eye Color: In rare cases, vitiligo may lead to changes in the color of the retina or iris.
While vitiligo itself is not painful or physically harmful, its visible nature can lead to psychological challenges, such as low self-esteem, anxiety, or depression.
Causes of Vitiligo
The exact cause of vitiligo is not fully understood, but researchers believe it involves a combination of genetic, autoimmune, and environmental factors. Below are some of the leading theories about what triggers this condition.
Autoimmune Response
One prevailing theory is that vitiligo occurs when the immune system mistakenly attacks and destroys melanocytes. This autoimmune response may be triggered by an underlying health condition or external factors, such as stress or exposure to certain chemicals.
Genetic Predisposition
Vitiligo tends to run in families, suggesting a genetic component. While having a family history of the condition does not guarantee that someone will develop it, it does increase the likelihood. Studies have identified several genes that may play a role in the development of vitiligo.
Oxidative Stress
Another possible cause is oxidative stress, which occurs when there is an imbalance between free radicals and antioxidants in the body. This imbalance can damage melanocytes, leading to their dysfunction or death. Environmental factors, such as exposure to industrial chemicals or ultraviolet radiation, may contribute to oxidative stress.
Neurogenic Factors
Some researchers propose that nerve endings in the skin may release substances that harm melanocytes. This neurogenic hypothesis is still being studied, but it offers another potential explanation for the development of vitiligo.
Types of Vitiligo
Vitiligo is generally classified into two main types based on the pattern and extent of depigmentation. Understanding these types can help guide treatment decisions and manage expectations.
Non-Segmental Vitiligo
Non-segmental vitiligo, also known as generalized vitiligo, is the most common form of the condition. It is characterized by symmetrical patches of depigmented skin that appear on both sides of the body. For example, if a patch develops on the left hand, a similar patch may appear on the right hand. Non-segmental vitiligo often progresses over time, with new patches appearing intermittently.
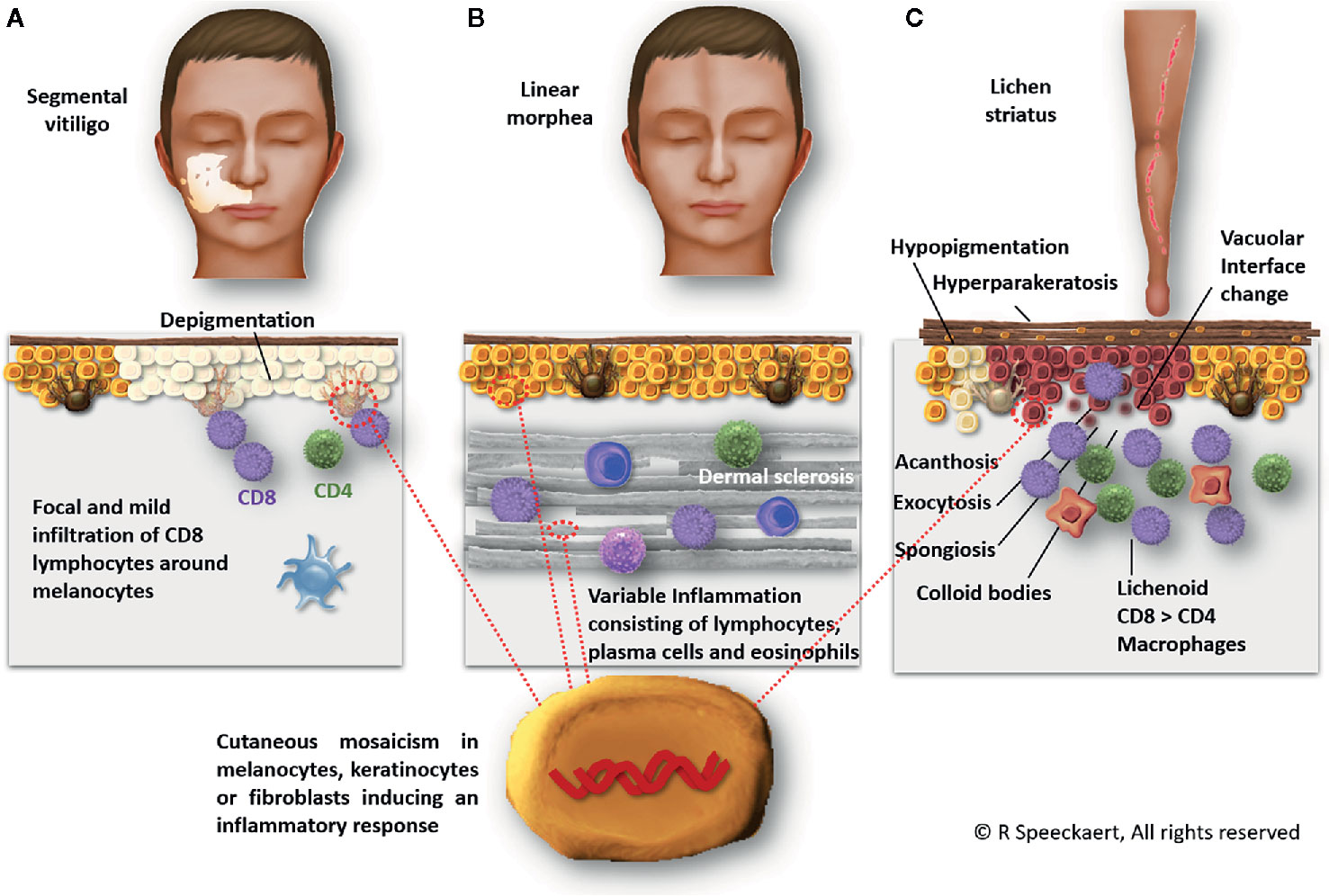
Segmental Vitiligo
Segmental vitiligo, on the other hand, affects only one side or segment of the body. This type tends to develop quickly and stabilize after a year or two. Unlike non-segmental vitiligo, segmental vitiligo is less likely to spread to other areas of the body.
Diagnosis of Vitiligo
Diagnosing vitiligo typically involves a physical examination and a review of the patient’s medical history. A dermatologist may use additional tests to confirm the diagnosis and rule out other conditions with similar symptoms.
Physical Examination
A healthcare provider will examine the affected areas of the skin under a special lamp called a Wood’s lamp. This device emits ultraviolet light, making depigmented patches more visible and helping to distinguish vitiligo from other skin conditions.
Medical History
The doctor will ask about the patient’s family history, any recent illnesses, or exposure to chemicals or stressors that could have triggered the condition. They may also inquire about any associated symptoms, such as premature graying or changes in eye color.
Biopsy and Blood Tests
In some cases, a skin biopsy may be performed to examine the melanocytes under a microscope. Blood tests may also be ordered to check for underlying autoimmune disorders, such as thyroid disease or diabetes, which are sometimes linked to vitiligo.
Treatment Options for Vitiligo
While there is no cure for vitiligo, several treatment options are available to help manage the condition and improve the appearance of affected skin. The choice of treatment depends on the severity of the condition, the patient’s preferences, and their overall health.
Topical Treatments
Corticosteroid creams are often prescribed to reduce inflammation and promote repigmentation in early-stage vitiligo. These creams work best when applied to small areas of depigmentation and are most effective when used consistently over several months.
Calcineurin inhibitors, such as tacrolimus and pimecrolimus, are alternative topical treatments that do not contain steroids. They are particularly useful for sensitive areas like the face and neck and may help restore some color to the skin.
Light Therapy
Phototherapy, or light therapy, involves exposing the skin to ultraviolet light under medical supervision. Narrowband UVB phototherapy is one of the most common forms of treatment and has been shown to stimulate melanocyte activity, leading to repigmentation.
PUVA therapy, which combines psoralen (a light-sensitizing medication) with UVA light, is another option. However, PUVA is less commonly used today due to the risk of side effects, such as sunburn and increased skin cancer risk.
Surgical Procedures
For individuals with stable vitiligo that does not respond to other treatments, surgical options may be considered. These include:
- Skin Grafting: Healthy skin is removed from an unaffected area and transplanted to the depigmented patches.
- Blister Grafting: Blisters are created on healthy skin using suction, and the tops of the blisters are transplanted to the affected areas.
- Melanocyte Transplantation: Melanocytes are harvested from a donor site and implanted into the depigmented areas.
Depigmentation
In cases where vitiligo affects a large portion of the body, some patients opt for depigmentation. This process involves applying a topical medication to remove the remaining pigment from unaffected areas, resulting in an even skin tone. Depigmentation is irreversible and requires careful consideration.
Living with Vitiligo
Managing vitiligo goes beyond medical treatments. Emotional and psychological support plays a crucial role in helping individuals cope with the condition and maintain a positive quality of life.
Emotional Impact
Vitiligo can significantly affect a person’s self-esteem and mental health. The visible nature of the condition may lead to feelings of embarrassment, social isolation, or discrimination. Seeking support from friends, family, or mental health professionals can be invaluable in navigating these challenges.
Lifestyle Adjustments
People with vitiligo are encouraged to take steps to protect their skin from sun damage, as depigmented areas are more vulnerable to sunburn. Wearing sunscreen, protective clothing, and hats can help minimize the risk of complications. Additionally, adopting a healthy lifestyle that includes a balanced diet, regular exercise, and stress management may support overall well-being.
Support Groups and Advocacy
Joining a support group or connecting with others who have vitiligo can provide a sense of community and understanding. Many organizations advocate for greater awareness and acceptance of vitiligo, working to dispel myths and reduce stigma surrounding the condition.
Emerging Research and Future Directions
Researchers continue to explore new treatments and therapies for vitiligo, offering hope for improved outcomes in the future. Advances in stem cell research, gene therapy, and immunology hold promise for addressing the root causes of the condition and promoting long-term repigmentation.
Additionally, efforts to raise awareness and educate the public about vitiligo are helping to foster a more inclusive and compassionate society. By challenging misconceptions and celebrating diversity, we can create a world where individuals with vitiligo feel empowered to embrace their unique beauty.





