Ventricular fibrillation, often abbreviated as VF, is a life-threatening heart condition that disrupts the normal electrical activity of the heart. This abnormal rhythm causes the heart’s lower chambers, known as the ventricles, to quiver instead of contracting effectively. As a result, blood circulation halts, leading to a medical emergency that requires immediate intervention. Understanding the causes, recognizing the symptoms, and knowing how to respond during an episode can save lives.
What is Ventricular Fibrillation?
Ventricular fibrillation occurs when the electrical signals in the heart become chaotic. Normally, the heart follows a precise sequence of electrical impulses that coordinate its contractions. In this condition, however, these signals are erratic, preventing the heart from pumping blood efficiently. Without prompt treatment, ventricular fibrillation can lead to sudden cardiac arrest and death within minutes.
The Role of the Heart’s Electrical System
The heart relies on its electrical system to maintain a steady rhythm. The sinoatrial node, located in the upper right chamber of the heart, acts as the natural pacemaker, initiating each heartbeat. These electrical signals travel through the atria (upper chambers) and then to the ventricles (lower chambers), causing them to contract in a synchronized manner. When ventricular fibrillation occurs, this synchronization breaks down, and the ventricles begin to twitch uncontrollably.
Causes of Ventricular Fibrillation
Several factors can trigger ventricular fibrillation. While some causes are related to pre-existing heart conditions, others may occur unexpectedly. Below are the most common causes:
Heart Attacks
A heart attack, also known as myocardial infarction, is one of the leading causes of ventricular fibrillation. During a heart attack, a blockage in the coronary arteries cuts off blood flow to a part of the heart muscle. This lack of oxygen can damage the heart tissue and disrupt its electrical activity, potentially leading to ventricular fibrillation.
Coronary Artery Disease
Coronary artery disease occurs when the arteries supplying blood to the heart become narrowed or blocked due to plaque buildup. Over time, this condition weakens the heart and increases the risk of abnormal rhythms, including ventricular fibrillation.
Cardiomyopathy
Cardiomyopathy refers to diseases of the heart muscle that make it harder for the heart to pump blood effectively. Certain types of cardiomyopathy, such as dilated or hypertrophic cardiomyopathy, can predispose individuals to ventricular fibrillation.
Electrolyte Imbalances
Electrolytes like potassium, sodium, calcium, and magnesium play a crucial role in maintaining the heart’s electrical stability. Abnormal levels of these electrolytes can interfere with the heart’s ability to conduct electrical signals properly, increasing the risk of ventricular fibrillation.
Drug Toxicity or Overdose
Certain medications, particularly those affecting the heart’s rhythm, can cause ventricular fibrillation if taken in excessive amounts or combined with other substances. Recreational drug use, such as cocaine or methamphetamine, can also trigger this condition.
Trauma or Injury
Severe trauma to the chest, such as from a car accident or electrocution, can damage the heart and disrupt its electrical system. In some cases, this damage may result in ventricular fibrillation.
Genetic Factors
Some individuals are born with genetic mutations that affect the heart’s electrical system. Conditions like long QT syndrome or Brugada syndrome increase the likelihood of developing ventricular fibrillation.
Symptoms of Ventricular Fibrillation
Ventricular fibrillation often strikes without warning, but there are signs that may indicate an impending episode. Recognizing these symptoms early can be critical for survival.
Sudden Collapse
One of the hallmark symptoms of ventricular fibrillation is a sudden loss of consciousness. When the heart stops pumping blood effectively, the brain does not receive enough oxygen, causing the person to collapse.
No Pulse or Breathing
In cases of ventricular fibrillation, the heart cannot maintain a regular rhythm, leading to a lack of pulse and breathing. If someone appears unresponsive and has no detectable pulse, it is essential to act quickly.
Chest Pain
Prior to an episode, some individuals may experience intense chest pain. This discomfort is often described as pressure, tightness, or a squeezing sensation in the chest.
Shortness of Breath
Difficulty breathing or feeling out of breath can occur before or during an episode of ventricular fibrillation. This symptom is typically accompanied by a rapid heartbeat.
Dizziness or Lightheadedness
A sudden drop in blood pressure caused by ineffective heart contractions can lead to dizziness or lightheadedness. These sensations may precede a full-blown episode.
Rapid or Irregular Heartbeat
An abnormally fast or irregular heartbeat, known as palpitations, may signal an underlying issue with the heart’s electrical system. If left untreated, this can progress to ventricular fibrillation.
Emergency Care for Ventricular Fibrillation
Ventricular fibrillation is a medical emergency that demands immediate attention. The sooner treatment begins, the better the chances of survival. Here are the key steps involved in providing emergency care:
Call for Help
If you suspect someone is experiencing ventricular fibrillation, call emergency services immediately. Time is of the essence, and professional medical assistance is required to stabilize the individual.
Begin Cardiopulmonary Resuscitation (CPR)
While waiting for help to arrive, start performing cardiopulmonary resuscitation. CPR involves chest compressions and rescue breaths to manually circulate blood and deliver oxygen to vital organs. Proper technique is crucial, so follow these guidelines:
- Place the heel of one hand on the center of the person’s chest.
- Place your other hand on top and interlock your fingers.
- Push hard and fast, aiming for a depth of about two inches and a rate of 100 to 120 compressions per minute.
- After 30 compressions, give two rescue breaths if trained to do so.
Use an Automated External Defibrillator (AED)
An automated external defibrillator is a portable device designed to restore a normal heart rhythm by delivering an electric shock. AEDs are widely available in public places and are easy to use, even for non-medical personnel. Follow these steps:
- Turn on the AED and follow the voice prompts.
- Attach the electrode pads to the person’s bare chest as instructed.
- Ensure no one is touching the person while the AED analyzes the heart rhythm.
- If advised, press the button to deliver a shock.
- Resume CPR until emergency responders arrive or the person regains consciousness.
Hospital Treatment
Once the individual reaches the hospital, healthcare providers will continue advanced life support measures. These may include:
- Administering medications to stabilize the heart rhythm.
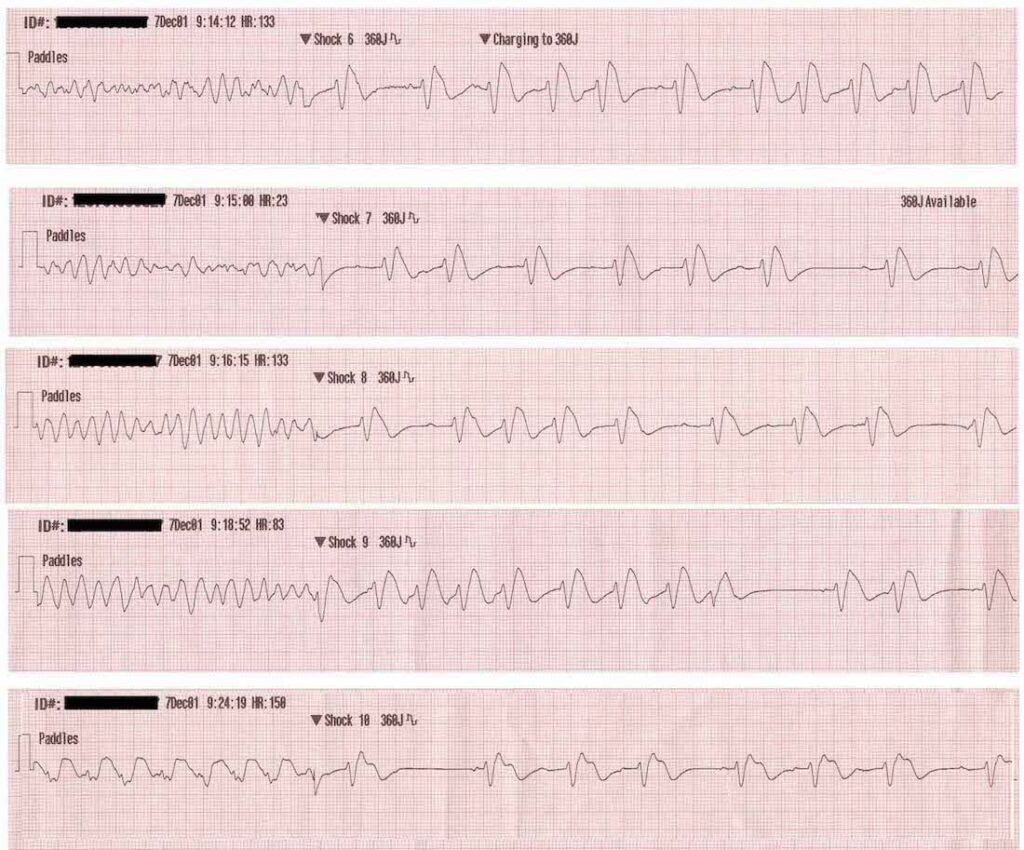
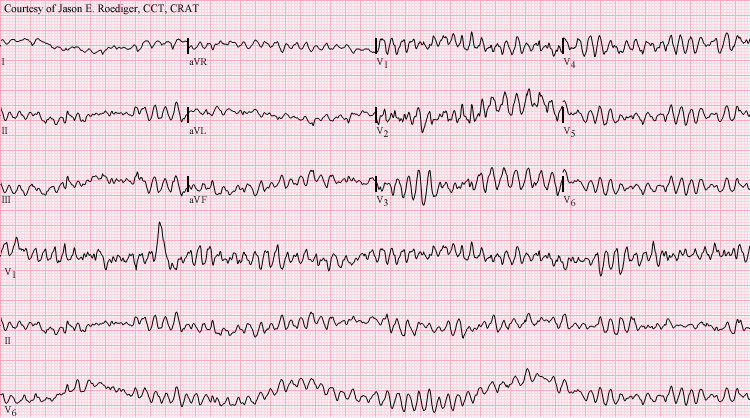
- Performing additional defibrillation attempts if necessary.
- Inserting a temporary pacemaker or implantable cardioverter-defibrillator to prevent future episodes.
- Conducting tests, such as an electrocardiogram or echocardiogram, to determine the underlying cause.
Post-Emergency Care
After surviving an episode of ventricular fibrillation, ongoing care is essential to reduce the risk of recurrence. This may involve:
- Taking prescribed medications, such as beta-blockers or antiarrhythmic drugs.
- Making lifestyle changes, including adopting a heart-healthy diet and exercising regularly.
- Managing underlying conditions, such as high blood pressure or diabetes.
- Attending regular follow-up appointments with a cardiologist.
Preventing Ventricular Fibrillation
While not all cases of ventricular fibrillation can be prevented, certain measures can significantly lower the risk. These include:
- Controlling risk factors such as smoking, obesity, and high cholesterol.
- Monitoring and managing chronic health conditions like hypertension and coronary artery disease.
- Avoiding excessive alcohol consumption and recreational drug use.
- Learning basic first aid and CPR techniques to assist others in emergencies.