Vasovagal syncope, often abbreviated as VVS, is a common condition characterized by a temporary loss of consciousness due to a sudden drop in blood flow to the brain. While it may sound alarming, this condition is generally harmless and can be managed effectively with proper understanding and lifestyle adjustments. This article explores the nature of vasovagal syncope, its triggers, and strategies for managing and preventing episodes.
Understanding Vasovagal Syncope
Vasovagal syncope occurs when the body overreacts to certain triggers, causing the heart rate and blood pressure to drop suddenly. This reaction leads to reduced blood flow to the brain, resulting in fainting. The term “vasovagal” refers to the involvement of the vagus nerve, which plays a key role in regulating heart rate and blood pressure.
The vagus nerve is part of the autonomic nervous system, which controls involuntary bodily functions such as breathing, digestion, and heart rate. When the vagus nerve is stimulated excessively, it can cause the heart to slow down and blood vessels to dilate, leading to a drop in blood pressure. This chain reaction is what causes a person to faint during an episode of vasovagal syncope.
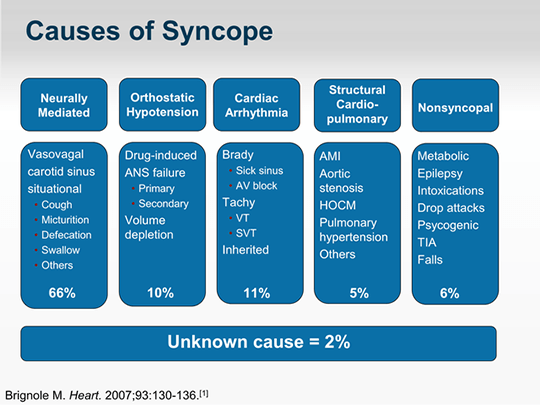
How Common Is Vasovagal Syncope?
Vasovagal syncope is one of the most common causes of fainting and can affect people of all ages. It is particularly prevalent among young adults and teenagers, although it can occur at any stage of life. Studies suggest that up to 40 percent of people will experience at least one episode of vasovagal syncope in their lifetime. While it is generally not life-threatening, repeated episodes can disrupt daily life and lead to anxiety or fear of fainting in public.
Triggers of Vasovagal Syncope
One of the defining features of vasovagal syncope is its association with specific triggers. These triggers vary from person to person, but some are more common than others. Understanding these triggers can help individuals identify situations that may lead to an episode and take preventive measures.
Emotional Stress and Anxiety
Strong emotions such as fear, stress, or anxiety can trigger vasovagal syncope. For example, witnessing a traumatic event, receiving unexpected bad news, or even experiencing intense excitement can overwhelm the nervous system and lead to fainting. Emotional triggers are particularly common in people who are highly sensitive to stress.
Painful or Uncomfortable Situations
- Blood Draws or Injections: Many people experience vasovagal syncope during medical procedures such as blood tests or vaccinations. The sight of blood or needles can activate the vagus nerve and cause fainting.
- Injuries: Severe pain from injuries, even if they are minor, can also act as a trigger.
Prolonged Standing
Standing for extended periods, especially in hot or crowded environments, can lead to vasovagal syncope. This is because standing for too long can cause blood to pool in the legs, reducing the amount of blood returning to the heart. As a result, blood pressure drops, and fainting may occur.
Dehydration and Hunger
Dehydration and low blood sugar levels can make the body more susceptible to vasovagal syncope. When the body lacks adequate fluids or nutrients, blood pressure can drop, increasing the risk of fainting. This is why fainting is more likely to occur during fasting or after intense physical activity without proper hydration.
Environmental Factors
Extreme temperatures, whether hot or cold, can also trigger vasovagal syncope. For instance, being in a hot room or wearing heavy clothing in warm weather can cause excessive sweating and dehydration, both of which contribute to fainting episodes.
Symptoms of Vasovagal Syncope
Before fainting occurs, individuals with vasovagal syncope often experience warning signs. Recognizing these symptoms can help prevent an episode by allowing the person to sit or lie down before losing consciousness. Common symptoms include:
- Dizziness or lightheadedness
- Nausea or stomach discomfort
- A feeling of warmth or sweating
- Blurred vision or tunnel vision
- Pale skin
- A rapid or slow heartbeat
These symptoms typically occur just before fainting and may last for a few seconds to several minutes. Once the person faints, they usually regain consciousness within a minute or two. Afterward, they may feel tired, confused, or disoriented for a short period.
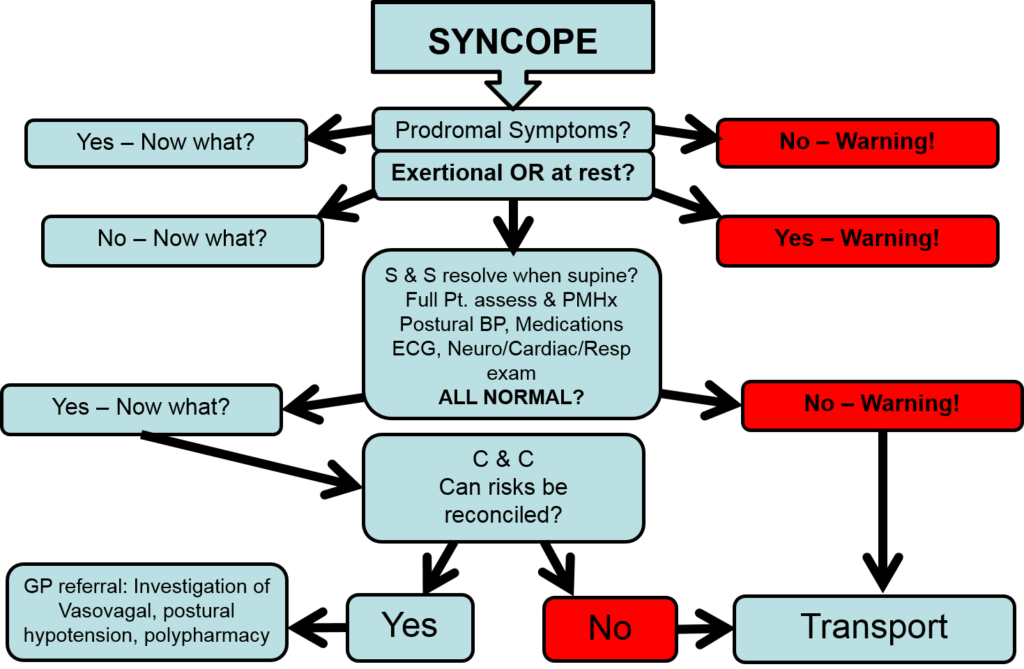
Diagnosing Vasovagal Syncope
If someone experiences frequent fainting episodes, it is important to consult a healthcare provider to rule out other potential causes. While vasovagal syncope is usually harmless, fainting can sometimes indicate a more serious underlying condition, such as heart problems or neurological disorders.
Medical History and Physical Examination
During the initial evaluation, a doctor will review the patient’s medical history and ask about the circumstances surrounding their fainting episodes. They will also perform a physical examination to check for any abnormalities in heart rate, blood pressure, or neurological function.
Diagnostic Tests
In some cases, additional tests may be needed to confirm the diagnosis and rule out other conditions. These tests may include:
- Electrocardiogram (ECG): This test measures the electrical activity of the heart to detect irregularities in heart rhythm.
- Tilt Table Test: During this test, the patient lies on a table that is tilted to simulate the effects of standing up. It helps determine whether fainting is caused by changes in posture.
- Blood Tests: Blood tests can identify issues such as anemia or low blood sugar, which may contribute to fainting.
Managing and Preventing Vasovagal Syncope
While vasovagal syncope cannot always be completely prevented, there are several strategies that can reduce the frequency and severity of episodes. These strategies focus on avoiding triggers, making lifestyle changes, and using specific techniques to manage symptoms.
Avoiding Known Triggers
Identifying and avoiding triggers is one of the most effective ways to prevent vasovagal syncope. For example:
- Stay hydrated by drinking plenty of water throughout the day.
- Eat regular meals to maintain stable blood sugar levels.
- Avoid standing for long periods, especially in hot or crowded environments.
- Use relaxation techniques to manage stress and anxiety.
Physical Maneuvers to Prevent Fainting
When warning signs of vasovagal syncope occur, certain physical maneuvers can help prevent fainting. These include:
- Lying Down: Lying flat on the back with the legs elevated can improve blood flow to the brain.
- Crossing Legs and Tensing Muscles: This technique increases blood pressure and can prevent fainting in some cases.
- Gripping Objects Tightly: Squeezing a stress ball or gripping the edge of a table can activate muscles and raise blood pressure.
Lifestyle Modifications
Making certain lifestyle changes can also reduce the likelihood of fainting episodes. These changes include:
- Wearing compression stockings to improve blood circulation in the legs.
- Avoiding alcohol and caffeine, which can dehydrate the body and lower blood pressure.
- Exercising regularly to improve cardiovascular health and circulation.
Medications and Other Treatments
In rare cases where lifestyle changes and preventive measures are not enough, medications may be prescribed to manage vasovagal syncope. These medications work by stabilizing blood pressure and heart rate. However, they are typically used only for individuals with severe or recurrent episodes.
Other treatments, such as biofeedback therapy or cognitive-behavioral therapy, may also be recommended for people who experience significant anxiety related to their condition. These therapies can help individuals develop coping mechanisms and reduce their fear of fainting.
When to Seek Medical Attention
While vasovagal syncope is usually harmless, certain situations warrant immediate medical attention. These include:
- Fainting during physical activity or exercise
- Fainting accompanied by chest pain, shortness of breath, or palpitations
- Frequent or unexplained fainting episodes
- Injuries sustained during a fainting episode
If any of these symptoms occur, it is important to seek medical care promptly to rule out serious underlying conditions.