Vascular dementia, often abbreviated as VaD, is a condition that affects the brain’s ability to function properly due to impaired blood flow. This type of dementia is the second most common form after Alzheimer’s disease and can significantly impact memory, thinking, and behavior. Understanding vascular dementia is essential for early detection, proper management, and improving the quality of life for those affected. In this article, we will explore the causes, symptoms, and care options available for individuals living with vascular dementia.
What is Vascular Dementia?
Vascular dementia occurs when there is reduced blood flow to the brain, leading to damage in brain cells. The brain relies on a constant supply of oxygen and nutrients delivered through blood vessels. When these vessels are blocked or damaged, it disrupts the brain’s ability to perform its functions effectively. Unlike other forms of dementia, vascular dementia often progresses in a stepwise manner, with periods of stability followed by sudden declines in cognitive abilities.
Types of Vascular Dementia
- Multi-infarct dementia: This type occurs when multiple small strokes damage areas of the brain over time.
- Subcortical vascular dementia: Also known as Binswanger’s disease, this form involves damage to the deeper parts of the brain, affecting movement and coordination.
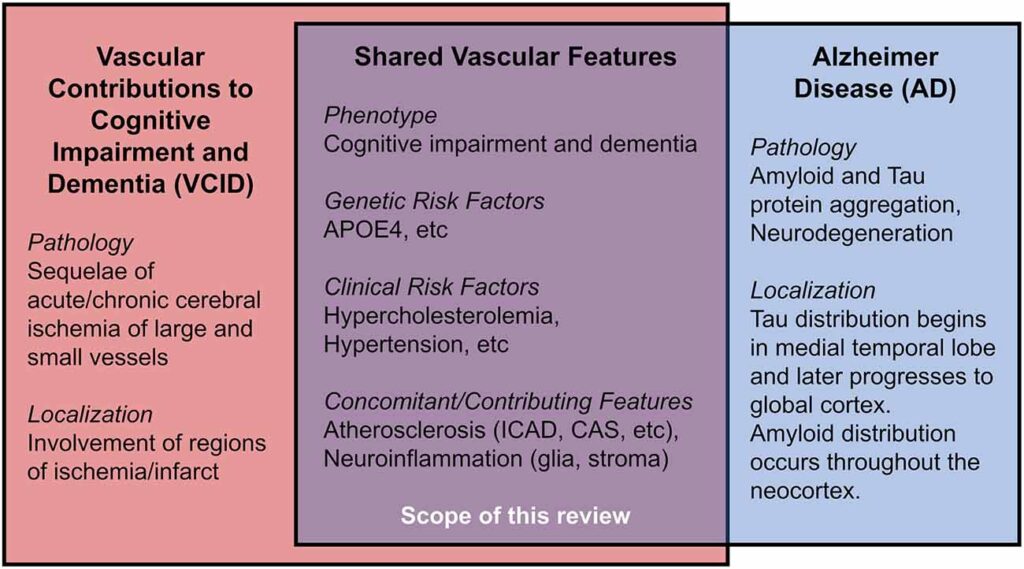
- Mixed dementia: This refers to cases where vascular dementia coexists with other types of dementia, such as Alzheimer’s disease.
Causes of Vascular Dementia
The primary cause of vascular dementia is the interruption of blood flow to the brain. Several underlying conditions and risk factors contribute to this disruption, including:
Stroke
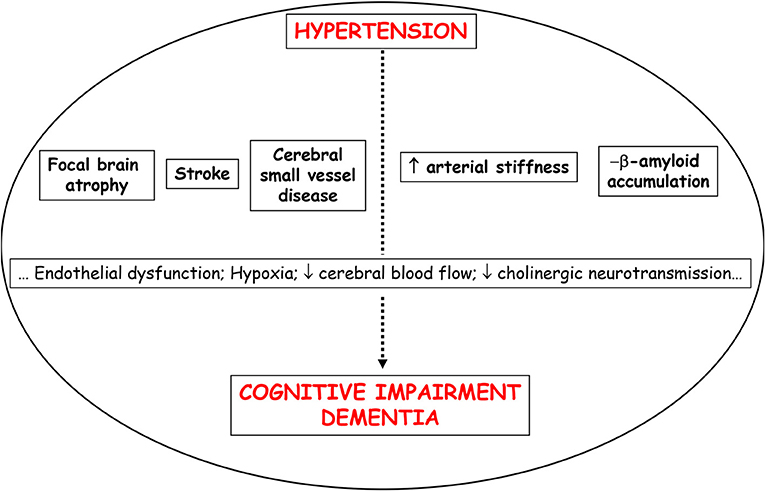
A stroke occurs when a blood vessel in the brain is blocked or bursts, cutting off the supply of oxygen and nutrients to brain cells. Strokes can lead to immediate cognitive decline and increase the risk of developing vascular dementia.
Small Vessel Disease
Small vessel disease refers to damage to the tiny blood vessels deep within the brain. This condition can result from high blood pressure, diabetes, or other cardiovascular issues. Over time, the cumulative damage can impair brain function and lead to dementia.
Heart Conditions
Certain heart conditions, such as atrial fibrillation, heart failure, or coronary artery disease, can increase the risk of vascular dementia. These conditions may cause blood clots or reduce the efficiency of blood flow to the brain.
Risk Factors
Several factors can elevate the risk of developing vascular dementia, including:
- High blood pressure
- Diabetes
- High cholesterol levels
- Smoking
- Obesity
- Lack of physical activity
- Family history of stroke or dementia
Symptoms of Vascular Dementia
The symptoms of vascular dementia can vary depending on the part of the brain affected and the severity of the damage. Common signs include:
Cognitive Decline
Individuals with vascular dementia often experience difficulties with memory, attention, and problem-solving. Unlike Alzheimer’s disease, memory loss may not be the first noticeable symptom. Instead, problems with planning, organizing, and decision-making are more prominent.
Language and Communication Issues
People with vascular dementia may struggle to find the right words during conversations or have difficulty understanding spoken or written language. This can lead to frustration and withdrawal from social interactions.
Physical Symptoms
In some cases, vascular dementia can cause physical symptoms such as unsteady gait, poor balance, or difficulty with coordination. These issues are particularly common in subcortical vascular dementia.
Mood and Behavioral Changes
Depression, apathy, irritability, and mood swings are frequent among individuals with vascular dementia. These changes can occur suddenly and may worsen over time.
Progression of Symptoms
Vascular dementia typically progresses in a stepwise pattern. After a stroke or other vascular event, there may be a noticeable decline in cognitive abilities, followed by periods of stability. However, repeated events can lead to further deterioration.
Diagnosis of Vascular Dementia
Diagnosing vascular dementia involves a comprehensive evaluation by healthcare professionals. The process includes:
Medical History and Physical Examination
A doctor will review the patient’s medical history, focusing on any past strokes, heart conditions, or risk factors. A physical examination helps identify signs of neurological impairment.
Cognitive Testing
Standardized tests assess memory, language, reasoning, and other cognitive functions. These assessments help determine the extent of cognitive decline and differentiate vascular dementia from other types of dementia.
Imaging Studies
Brain imaging techniques, such as magnetic resonance imaging or computed tomography scans, are used to detect abnormalities in the brain, such as areas of dead tissue caused by strokes or small vessel disease.
Laboratory Tests
Blood tests may be conducted to rule out other potential causes of cognitive impairment, such as vitamin deficiencies or thyroid disorders.
Care Options for Vascular Dementia
While there is no cure for vascular dementia, various treatments and care strategies can help manage symptoms and improve quality of life. These options focus on addressing underlying health conditions, providing support for daily activities, and enhancing emotional well-being.
Medications
Although no specific drugs are approved to treat vascular dementia, certain medications can help manage symptoms or slow the progression of the disease:
- Blood pressure medications: Controlling hypertension reduces the risk of further strokes and slows cognitive decline.
- Cholesterol-lowering drugs: Statins may be prescribed to lower cholesterol levels and protect blood vessels.
- Anticoagulants: For individuals with atrial fibrillation, these medications prevent blood clots and reduce the risk of stroke.
- Antidepressants: These can help alleviate symptoms of depression and anxiety associated with vascular dementia.
Lifestyle Modifications
Making healthy lifestyle choices can significantly impact the progression of vascular dementia:
- Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins supports overall health and reduces the risk of cardiovascular disease.
- Exercise: Regular physical activity improves circulation, strengthens the heart, and enhances cognitive function.
- Smoking cessation: Quitting smoking lowers the risk of stroke and other vascular complications.
- Alcohol moderation: Limiting alcohol consumption helps maintain brain health.
Therapies and Support
Various therapies can assist individuals with vascular dementia in maintaining independence and coping with challenges:
- Occupational therapy: Helps patients adapt to changes in their abilities and learn new ways to perform daily tasks.
- Speech therapy: Improves communication skills and addresses language difficulties.
- Counseling: Provides emotional support for both patients and caregivers, helping them navigate the challenges of living with dementia.
Support for Caregivers
Caring for someone with vascular dementia can be physically and emotionally demanding. It is crucial for caregivers to seek support and resources to prevent burnout:
- Respite care: Offers temporary relief for caregivers by providing professional assistance.
- Support groups: Connect caregivers with others facing similar challenges, offering a sense of community and shared experiences.
- Educational programs: Teach caregivers about the disease and effective caregiving strategies.
Preventing Vascular Dementia
While not all cases of vascular dementia can be prevented, adopting a proactive approach to health can significantly reduce the risk:
- Manage chronic conditions like high blood pressure, diabetes, and high cholesterol.
- Engage in regular physical activity and maintain a healthy weight.
- Eat a nutritious diet low in saturated fats and sodium.
- Avoid smoking and limit alcohol intake.
- Stay socially active and mentally engaged through hobbies, puzzles, and social interactions.