Vaginitis, often abbreviated as VI, is a common condition that affects millions of women worldwide. It refers to the inflammation or infection of the vagina, leading to discomfort, irritation, and other symptoms. This article delves into the various aspects of this condition, including its causes, types, symptoms, and available treatments. By understanding these elements, individuals can better manage their health and seek appropriate care when needed.
What Is Vaginitis?
Vaginitis is a broad term used to describe any condition that causes inflammation or infection in the vaginal area. The condition may result from a variety of factors, including infections, hormonal changes, or irritants. While it is most commonly associated with itching, burning, and unusual discharge, vaginitis can manifest differently depending on its underlying cause.
Common Causes of Vaginitis
The causes of vaginitis are diverse, ranging from bacterial imbalances to external irritants. Below are some of the most common causes:
- Bacterial Imbalance: The vagina naturally contains a balance of bacteria. When this balance is disrupted, harmful bacteria can overgrow, leading to infection.
- Fungal Infections: Yeast infections are a prevalent type of vaginitis caused by an overgrowth of the fungus Candida.
- Parasitic Infections: Trichomoniasis, a sexually transmitted infection, can also lead to vaginitis.
- Hormonal Changes: Fluctuations in hormone levels, particularly during pregnancy, menopause, or menstruation, can increase the risk of developing vaginitis.
- Irritants: Certain soaps, detergents, perfumes, and other chemical substances can irritate the vaginal lining, causing inflammation.
- Allergic Reactions: Some individuals may experience vaginitis due to an allergic reaction to latex condoms, spermicides, or other products.
Types of Vaginitis
There are several distinct types of vaginitis, each with its own set of characteristics. Understanding these types is essential for accurate diagnosis and treatment.
Bacterial Vaginosis
Bacterial vaginosis occurs when there is an overgrowth of harmful bacteria in the vagina. This condition often results in a fishy-smelling discharge and is more common in women who are sexually active. Although it is not classified as a sexually transmitted infection, having multiple sexual partners or frequent intercourse can increase the risk of developing bacterial vaginosis.
Yeast Infection
A yeast infection, also known as candidiasis, is caused by an overgrowth of the fungus Candida. This type of vaginitis is characterized by thick, white discharge, intense itching, and redness around the vaginal area. Factors such as antibiotic use, diabetes, and a weakened immune system can contribute to the development of yeast infections.
Trichomoniasis
Trichomoniasis is a sexually transmitted infection caused by a parasite. It often leads to frothy, yellow-green discharge, along with itching and irritation. Unlike other types of vaginitis, trichomoniasis requires treatment for both the infected individual and their sexual partner to prevent reinfection.
Atrophic Vaginitis
Atrophic vaginitis occurs due to a decrease in estrogen levels, which typically happens during menopause. The reduced estrogen levels cause thinning and inflammation of the vaginal walls, leading to symptoms such as dryness, burning, and pain during intercourse.
Contact Dermatitis
Contact dermatitis is a form of vaginitis caused by an allergic reaction or irritation from external substances. Common culprits include scented soaps, bubble baths, and laundry detergents. Symptoms may include redness, swelling, and itching in the affected area.
Symptoms of Vaginitis
The symptoms of vaginitis can vary depending on the underlying cause. However, some common signs and symptoms include:
- Abnormal vaginal discharge (color, consistency, or odor may differ)
- Vaginal itching or irritation
- Burning sensation during urination or intercourse
- Redness or swelling of the vulva
- Pain or discomfort in the pelvic area
It is important to note that some individuals may experience mild symptoms or no symptoms at all, especially in cases of bacterial vaginosis. If left untreated, certain types of vaginitis can lead to complications, such as pelvic inflammatory disease or increased susceptibility to sexually transmitted infections.
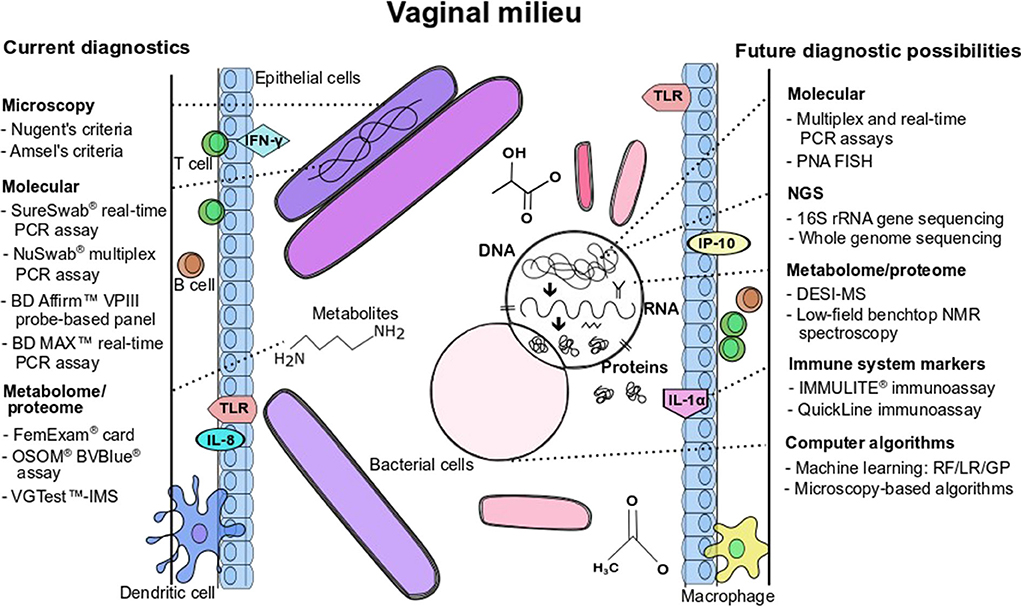
Diagnosis of Vaginitis
To diagnose vaginitis, healthcare providers typically begin by taking a detailed medical history and conducting a physical examination. During the examination, they may collect a sample of vaginal discharge for laboratory analysis. This helps determine the specific cause of the inflammation or infection, allowing for targeted treatment.
In some cases, additional tests may be necessary, such as pH testing or DNA probes, to confirm the diagnosis. Accurate diagnosis is crucial, as different types of vaginitis require different treatment approaches.
Treatment Options for Vaginitis
Treatment for vaginitis depends on the underlying cause and severity of the condition. Below are some common treatment options for each type of vaginitis:
Treatment for Bacterial Vaginosis
Bacterial vaginosis is typically treated with antibiotics, either in oral form or as a topical gel. Metronidazole and clindamycin are two commonly prescribed medications for this condition. It is essential to complete the full course of antibiotics, even if symptoms improve, to prevent recurrence.
Treatment for Yeast Infection
For yeast infections, antifungal medications are the primary treatment. These medications are available in various forms, including creams, suppositories, and oral tablets. Over-the-counter options are often effective for mild cases, but severe or recurrent infections may require prescription-strength treatment.
Treatment for Trichomoniasis
Trichomoniasis is treated with antibiotics, usually metronidazole or tinidazole. Both the infected individual and their sexual partner must undergo treatment to prevent reinfection. Sexual activity should be avoided until both partners have completed the treatment and are free of symptoms.
Treatment for Atrophic Vaginitis
Atrophic vaginitis is often managed with estrogen therapy. This can be administered in the form of vaginal creams, tablets, or rings. Estrogen therapy helps restore the natural balance of the vaginal environment, alleviating symptoms such as dryness and irritation.
Treatment for Contact Dermatitis
For contact dermatitis, the primary treatment involves identifying and avoiding the irritant or allergen causing the reaction. Topical corticosteroids or antihistamines may be prescribed to reduce inflammation and relieve itching.
Prevention of Vaginitis
While not all cases of vaginitis can be prevented, certain measures can reduce the risk of developing this condition:
- Maintain good hygiene by washing the genital area with water and avoiding harsh soaps or scented products.
- Wear breathable cotton underwear and avoid tight-fitting clothing.
- Practice safe sex by using condoms and limiting the number of sexual partners.
- Avoid douching, as it can disrupt the natural balance of bacteria in the vagina.
- Stay hydrated and maintain a healthy diet to support overall immune function.
When to Seek Medical Attention
While mild cases of vaginitis can often be managed at home, certain situations warrant immediate medical attention. These include:
- Symptoms that persist despite over-the-counter treatment
- Severe pain or discomfort
- Fever or chills accompanying vaginal symptoms
- Unusual or foul-smelling discharge
- Recurrent episodes of vaginitis
Seeking prompt medical care ensures accurate diagnosis and appropriate treatment, reducing the risk of complications.