Uterine fibroids, also known as leiomyomas or myomas, are noncancerous growths that develop in or on the muscular walls of the uterus. These growths are quite common among women of reproductive age and can vary significantly in size, number, and location. While many women with uterine fibroids experience no symptoms, others may face challenges such as heavy menstrual bleeding, pelvic pain, or fertility issues. Understanding the nature of these growths, their types, associated symptoms, and available treatments is crucial for managing them effectively.
What Are Uterine Fibroids?
Uterine fibroids are benign tumors that originate from the smooth muscle tissue of the uterus. They are made up of muscle cells and fibrous connective tissue. Although they are not cancerous and rarely develop into cancer, fibroids can cause significant discomfort and complications for some women. The exact cause of fibroids remains unclear, but several factors, including hormonal influences and genetic predisposition, are believed to play a role in their development.
Risk Factors for Developing Uterine Fibroids
- Age: Women in their thirties and forties are more likely to develop fibroids.
- Family History: A family history of fibroids increases the likelihood of developing them.
- Hormonal Influences: Estrogen and progesterone, hormones that regulate the menstrual cycle, appear to promote the growth of fibroids.
- Obesity: Being overweight or obese is associated with an increased risk of fibroids.
- Diet: Diets high in red meat and low in green vegetables may contribute to fibroid development.
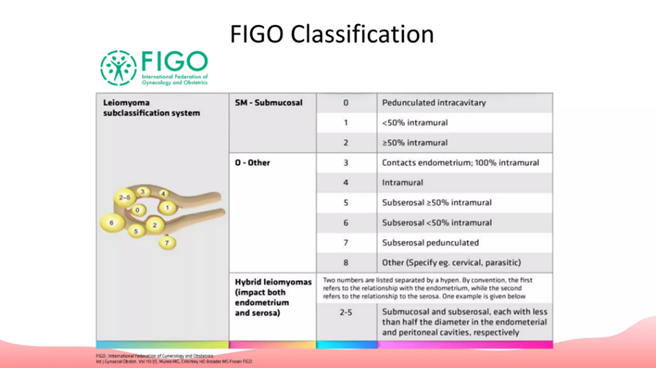
Types of Uterine Fibroids
Uterine fibroids are classified based on their location within or on the uterus. Each type has unique characteristics and may cause different symptoms.
Intramural Fibroids
Intramural fibroids are the most common type and grow within the muscular wall of the uterus. They can expand and distort the shape of the uterus, leading to symptoms such as heavy menstrual bleeding, pelvic pressure, and frequent urination.
Subserosal Fibroids
Subserosal fibroids develop on the outer surface of the uterus and can grow quite large. Because they protrude outward, they may press against nearby organs, causing back pain, constipation, or a feeling of fullness in the lower abdomen.
Submucosal Fibroids
Submucosal fibroids grow just beneath the inner lining of the uterus and project into the uterine cavity. Even small submucosal fibroids can cause significant symptoms, including heavy menstrual bleeding, prolonged periods, and difficulty conceiving.
Pedunculated Fibroids
Pedunculated fibroids are attached to the uterus by a stalk-like structure. They can be either subserosal or submucosal, depending on whether they grow outward or inward. These fibroids may cause sharp, intermittent pain if the stalk becomes twisted.
Symptoms of Uterine Fibroids
The symptoms of uterine fibroids vary widely depending on their size, number, and location. Some women with fibroids experience no symptoms at all, while others may face debilitating effects. Below are the most common symptoms associated with fibroids:
Heavy Menstrual Bleeding
One of the hallmark symptoms of fibroids is heavy menstrual bleeding, which can lead to anemia if left untreated. Women may notice that their periods last longer than usual or require frequent changes of sanitary products.
Pelvic Pain and Pressure
Fibroids can cause a sensation of fullness or pressure in the pelvic region. This discomfort may worsen over time as the fibroids grow larger.
Frequent Urination
Large fibroids, especially those located near the bladder, can press against it, leading to frequent urination or difficulty emptying the bladder completely.
Pain During Intercourse
Some women with fibroids experience pain or discomfort during sexual intercourse, particularly if the fibroids are located near the cervix or within the uterine cavity.
Infertility and Pregnancy Complications
In certain cases, fibroids can interfere with fertility by obstructing the fallopian tubes or distorting the uterine cavity. They may also increase the risk of complications during pregnancy, such as miscarriage or preterm labor.
Diagnosis of Uterine Fibroids
Diagnosing uterine fibroids typically involves a combination of medical history evaluation, physical examination, and imaging tests. Early detection is essential for effective management.
Physical Examination
A healthcare provider may detect fibroids during a routine pelvic exam. Large fibroids can often be felt as irregularities in the shape or size of the uterus.
Ultrasound Imaging
An ultrasound is one of the most common diagnostic tools used to identify fibroids. It provides detailed images of the uterus and helps determine the size, number, and location of the growths.
Magnetic Resonance Imaging (MRI)
In some cases, an MRI may be recommended to obtain more detailed information about the fibroids. This imaging technique is particularly useful for planning surgical interventions.
Hysteroscopy
A hysteroscopy involves inserting a thin, lighted tube through the vagina and cervix to examine the inside of the uterus. This procedure can help identify submucosal fibroids and other abnormalities.
Treatment Options for Uterine Fibroids
Treatment for uterine fibroids depends on the severity of symptoms, the size and location of the fibroids, and the patient’s age and desire for future fertility. There are both non-surgical and surgical options available.
Watchful Waiting
For women with asymptomatic fibroids, watchful waiting may be the best approach. Regular monitoring through check-ups and imaging tests ensures that any changes in the fibroids are detected early.
Medications
Several medications can help manage the symptoms of fibroids or shrink them temporarily. These include:
- Hormonal Birth Control: Oral contraceptives or progestin-releasing intrauterine devices can help regulate menstrual cycles and reduce heavy bleeding.
- Gonadotropin-Releasing Hormone Agonists: These medications lower estrogen levels, causing fibroids to shrink. However, they are typically used for short-term treatment due to potential side effects.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Over-the-counter pain relievers like ibuprofen can alleviate mild pelvic pain associated with fibroids.
Minimally Invasive Procedures
For women seeking alternatives to surgery, minimally invasive procedures offer effective solutions:
- Uterine Artery Embolization: This procedure blocks the blood supply to the fibroids, causing them to shrink.
- Endometrial Ablation: This technique destroys the lining of the uterus to reduce heavy menstrual bleeding.
- Myomectomy: A myomectomy involves surgically removing the fibroids while preserving the uterus. It is often recommended for women who wish to maintain their fertility.
Surgical Interventions
In severe cases, surgery may be necessary to remove the fibroids or the entire uterus:
- Hysterectomy: A hysterectomy involves the removal of the entire uterus and is considered a permanent solution for fibroids. It is typically reserved for women who do not wish to have children in the future.
- Laparoscopic Surgery: This minimally invasive surgical technique uses small incisions and specialized tools to remove fibroids.
Emerging Treatments
Researchers are continually exploring new treatments for fibroids, including focused ultrasound surgery and novel drug therapies. These innovations aim to provide less invasive and more targeted options for women with fibroids.
Lifestyle Changes to Manage Symptoms
In addition to medical treatments, certain lifestyle changes can help alleviate the symptoms of fibroids:
- Dietary Adjustments: Consuming a diet rich in fruits, vegetables, and whole grains while reducing red meat intake may help manage fibroid symptoms.
- Exercise: Regular physical activity can improve overall health and potentially reduce the risk of fibroid growth.
- Stress Management: Techniques such as yoga, meditation, and deep breathing can help reduce stress, which may indirectly benefit women with fibroids.