Ulcerative colitis, often abbreviated as UC, is a chronic inflammatory condition that primarily affects the large intestine, also known as the colon. This disease falls under the umbrella of inflammatory bowel diseases and can significantly impact a person’s quality of life. Understanding its causes, recognizing its symptoms, and exploring treatment options are crucial for managing this condition effectively.
What is Ulcerative Colitis?
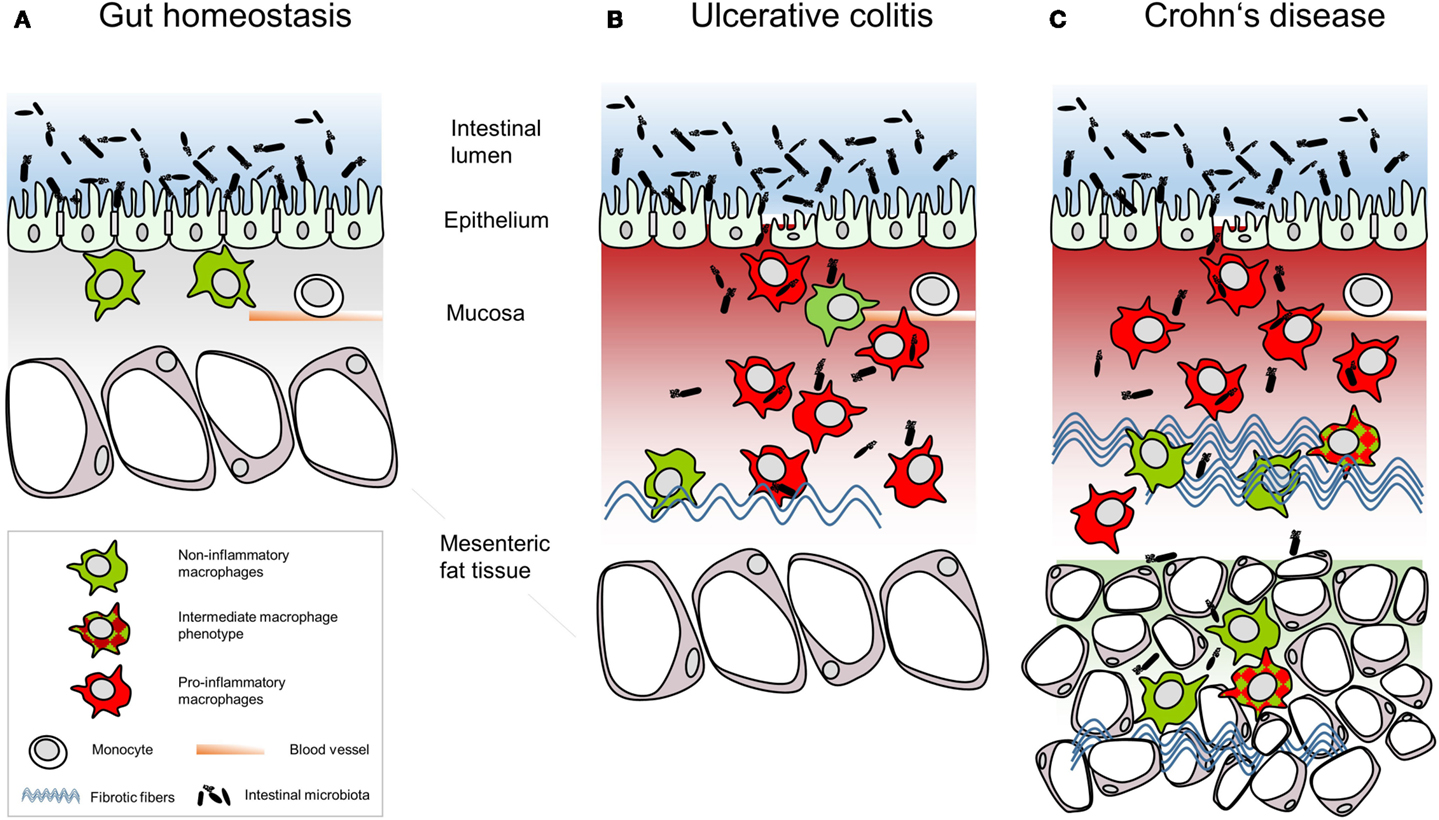
Ulcerative colitis is a type of inflammatory bowel disease characterized by inflammation and ulcers in the lining of the colon and rectum. Unlike other gastrointestinal disorders, ulcerative colitis specifically targets the innermost lining of the large intestine. The inflammation typically begins in the rectum and may spread continuously to other parts of the colon. It does not affect the small intestine, except in rare cases where it might involve the lower part, known as the terminal ileum.
This condition follows a pattern of flare-ups and remissions. During flare-ups, individuals experience active symptoms, while periods of remission bring relief from these symptoms. The severity and duration of flare-ups vary from person to person, making it a highly individualized disease.
Causes of Ulcerative Colitis
The exact cause of ulcerative colitis remains unknown, but researchers believe that it results from a combination of genetic, environmental, and immune system factors. Here’s a closer look at the potential causes:
Immune System Malfunction
One prevailing theory suggests that ulcerative colitis occurs when the immune system mistakenly attacks healthy cells in the digestive tract. Normally, the immune system fights off harmful bacteria and viruses. However, in people with this condition, the immune response is overactive and targets the lining of the colon, causing inflammation and ulcers.
Genetic Predisposition
Family history plays a significant role in the development of ulcerative colitis. Studies have shown that individuals with a close relative, such as a parent or sibling, who has the condition are at a higher risk of developing it themselves. Certain genes have been identified as potentially increasing susceptibility to the disease.
Environmental Triggers
Environmental factors, such as diet, stress, and exposure to certain medications or infections, may trigger or worsen symptoms in individuals predisposed to ulcerative colitis. For instance, smoking has been linked to an increased risk of developing the condition, although quitting smoking can sometimes lead to flare-ups in those already diagnosed.
Gut Microbiome Imbalance
The gut microbiome, which consists of trillions of microorganisms living in the digestive tract, plays a critical role in maintaining health. An imbalance in these microorganisms, known as dysbiosis, may contribute to the development of ulcerative colitis. Researchers are actively studying how changes in the gut microbiome influence the onset and progression of the disease.
Symptoms of Ulcerative Colitis
The symptoms of ulcerative colitis can range from mild to severe and often depend on the extent and location of inflammation within the colon. Some common symptoms include:
- Diarrhea: Frequent loose stools, often accompanied by blood or pus, are a hallmark symptom of this condition.
- Abdominal Pain: Cramping and pain in the abdomen are common, especially during flare-ups.
- Rectal Bleeding: Blood in the stool or during bowel movements is a frequent occurrence.
- Urgency to Defecate: Individuals may feel an uncontrollable urge to have a bowel movement.
- Fatigue: Chronic fatigue and low energy levels are often reported by those with ulcerative colitis.
- Weight Loss: Unintended weight loss can occur due to reduced appetite or difficulty absorbing nutrients.
- Fever: Low-grade fevers may accompany severe flare-ups.
In addition to these gastrointestinal symptoms, ulcerative colitis can also cause extraintestinal manifestations, meaning symptoms that affect other parts of the body. These may include joint pain, skin rashes, eye inflammation, and liver disorders.
Types of Ulcerative Colitis
Ulcerative colitis can manifest in different forms, depending on the area of the colon affected. Understanding the type of ulcerative colitis is essential for tailoring treatment plans. The main types include:
Ulcerative Proctitis
This is the mildest form of the condition, where inflammation is limited to the rectum. Symptoms are often less severe compared to other types, and individuals may experience rectal bleeding and urgency to defecate.
Proctosigmoiditis
In this type, inflammation extends from the rectum to the lower part of the colon, known as the sigmoid colon. Symptoms may include bloody diarrhea, abdominal cramps, and tenesmus, which is the sensation of needing to pass stool despite having an empty bowel.
Left-Sided Colitis
Left-sided colitis involves inflammation that extends from the rectum through the descending colon, located on the left side of the abdomen. Symptoms may include bloody diarrhea, pain on the left side of the abdomen, and weight loss.
Pancolitis
Pancolitis affects the entire colon and is considered one of the most severe forms of ulcerative colitis. Symptoms can be debilitating and include frequent bloody diarrhea, severe abdominal pain, fatigue, and significant weight loss.
Fulminant Colitis
This is a rare but life-threatening form of ulcerative colitis that causes extreme inflammation and damage to the entire colon. Fulminant colitis requires immediate medical attention and may necessitate surgery.
Treatment Options for Ulcerative Colitis
While there is no cure for ulcerative colitis, various treatments aim to reduce inflammation, manage symptoms, and achieve long-term remission. Treatment plans are highly individualized and depend on the severity of the condition, the affected area of the colon, and the patient’s overall health. Common treatment approaches include:
Medications
Several classes of medications are used to manage ulcerative colitis:
- Aminosalicylates: These anti-inflammatory drugs, such as sulfasalazine and mesalamine, are often prescribed for mild to moderate cases.
- Corticosteroids: Steroids like prednisone are used to control severe flare-ups but are not suitable for long-term use due to potential side effects.
- Immunomodulators: Medications such as azathioprine and methotrexate help suppress the immune system to reduce inflammation.
- Biologics: These advanced therapies target specific proteins involved in the inflammatory process. Examples include infliximab and adalimumab.
Dietary and Lifestyle Changes
Although diet does not cause ulcerative colitis, certain foods can exacerbate symptoms. A personalized diet plan, developed with the help of a healthcare provider or nutritionist, can help manage the condition. Common dietary recommendations include:
- Avoiding high-fiber foods during flare-ups
- Limiting dairy products if lactose intolerance is present
- Staying hydrated to prevent dehydration caused by diarrhea
- Eating smaller, more frequent meals
In addition to dietary adjustments, lifestyle changes such as regular exercise, stress management techniques, and adequate sleep can improve overall well-being and reduce symptom severity.
Surgery
In cases where medications fail to control symptoms or complications arise, surgery may be necessary. The most common surgical procedure for ulcerative colitis is a proctocolectomy, which involves removing the colon and rectum. After surgery, patients may require an ileostomy or an internal pouch-anal anastomosis to restore bowel function.
Alternative Therapies
Some individuals explore complementary and alternative therapies to supplement conventional treatments. These may include acupuncture, herbal supplements, and probiotics. While some people report benefits, it is essential to consult a healthcare provider before trying any alternative treatments, as they may interact with prescribed medications.
Complications of Ulcerative Colitis
If left untreated or poorly managed, ulcerative colitis can lead to serious complications, including:
- Severe bleeding
- Perforation of the colon
- Toxic megacolon, a dangerous enlargement of the colon
- An increased risk of colorectal cancer
- Osteoporosis due to long-term corticosteroid use
- Liver disease
Regular monitoring and adherence to treatment plans are crucial for minimizing the risk of complications.
Living with Ulcerative Colitis
Managing ulcerative colitis requires a proactive approach to healthcare. Building a strong support network, staying informed about the condition, and working closely with healthcare providers can empower individuals to take control of their health. Support groups, both in-person and online, offer valuable resources and a sense of community for those navigating life with this chronic illness.





