Trichinosis, also known as trichinellosis, is a parasitic disease caused by the roundworm Trichinella spiralis. This condition, abbreviated as TRS, occurs when humans consume meat contaminated with the larvae of this parasite. While it is relatively rare in developed countries due to strict food safety regulations, trichinosis remains a significant health concern in regions where undercooked or raw meat is consumed. Below, we explore the causes, symptoms, diagnosis, and treatment of this roundworm infection.
Causes of Trichinosis
Trichinosis is primarily caused by the consumption of meat that contains the larvae of the roundworm Trichinella spiralis. These microscopic worms can infect a variety of animals, but the most common sources of human infection are pork, wild game, and bear meat. The lifecycle of the parasite involves two stages: the adult worm and the larval form.
How the Parasite Infects Humans
The infection begins when a person eats meat that has not been cooked thoroughly. The meat contains cysts, which are protective capsules that house the larvae of the roundworm. Once inside the human digestive system, the stomach acid and enzymes break down the cysts, releasing the larvae. These larvae then mature into adult worms in the small intestine.
- Adult Worms: The adult worms mate in the small intestine, producing new larvae.
- Larvae Migration: The newly produced larvae penetrate the intestinal wall and enter the bloodstream, traveling to various muscles throughout the body.
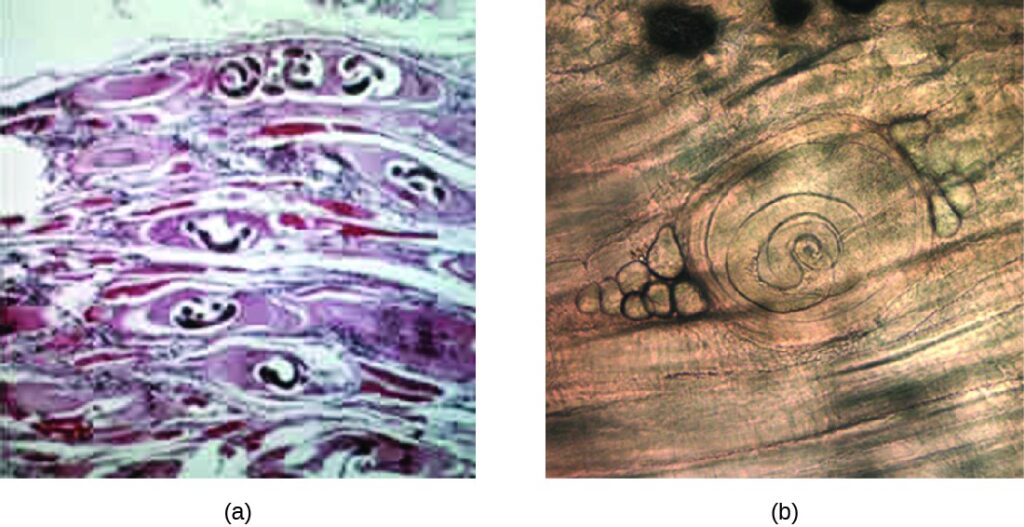
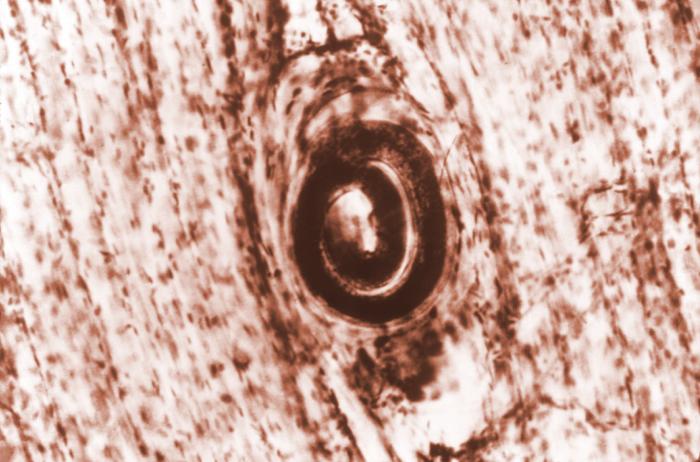
- Cyst Formation: Once in the muscles, the larvae encyst themselves, remaining dormant for extended periods unless treated.
Risk Factors for Trichinosis
Certain behaviors and practices increase the risk of contracting trichinosis:
- Eating raw or undercooked pork, wild game, or bear meat.
- Consuming homemade sausages or cured meats that have not been properly processed.
- Hunting and consuming wild animals without proper cooking methods.
- Lack of awareness about safe food handling and preparation.
Symptoms of Trichinosis
The symptoms of trichinosis vary depending on the stage of the infection and the number of parasites ingested. Some individuals may experience mild symptoms, while others may develop severe complications. The infection typically progresses through two main phases: the intestinal phase and the muscle invasion phase.
Intestinal Phase Symptoms
During the first week after ingestion, the adult worms multiply in the intestines, causing gastrointestinal symptoms. These may include:
- Nausea and vomiting.
- Diarrhea or constipation.
- Abdominal pain and cramping.
- Fatigue and weakness.
Muscle Invasion Phase Symptoms
As the larvae migrate to the muscles, systemic symptoms begin to appear, usually within two to eight weeks after infection. These symptoms are often more severe and may include:
- Fever and chills.
- Muscle pain and tenderness, particularly in the jaw, neck, shoulders, and lower back.
- Swelling around the eyes and face.
- Difficulty breathing or swallowing.
- Rashes or skin lesions.
Potential Complications
If left untreated, trichinosis can lead to serious complications, including:
- Inflammation of the heart muscle, leading to myocarditis.
- Central nervous system involvement, resulting in encephalitis or meningitis.
- Breathing difficulties due to diaphragm muscle involvement.
- Chronic muscle pain and weakness.
Diagnosis of Trichinosis
Diagnosing trichinosis can be challenging because its symptoms mimic those of other illnesses, such as the flu or food poisoning. A combination of clinical evaluation, laboratory tests, and imaging studies is often required to confirm the presence of the parasite.
Clinical Evaluation
A healthcare provider will begin by taking a detailed medical history, focusing on recent dietary habits and exposure to raw or undercooked meat. They will also conduct a physical examination to check for signs of muscle inflammation, swelling, or tenderness.
Laboratory Tests
Several laboratory tests can help diagnose trichinosis:
- Blood Tests: Elevated levels of white blood cells and eosinophils, a type of immune cell, are common indicators of parasitic infections.
- Serology Tests: These detect specific antibodies produced by the immune system in response to the roundworm.
- Muscle Biopsy: In some cases, a small sample of muscle tissue may be taken to identify encysted larvae under a microscope.
Imaging Studies
Imaging techniques, such as magnetic resonance imaging or computed tomography scans, may be used to assess muscle inflammation and damage caused by the larvae.
Treatment of Trichinosis
Early diagnosis and treatment are crucial for managing trichinosis effectively. While there is no specific cure for the infection, medications and supportive care can alleviate symptoms and prevent complications.
Medications
Antiparasitic drugs are the primary treatment for trichinosis. These medications target the adult worms and larvae, reducing their numbers and preventing further damage. Commonly prescribed drugs include:
- Albendazole: This drug is effective against both adult worms and larvae. It works by disrupting the parasite’s ability to absorb glucose, leading to its death.
- Mebendazole: Similar to albendazole, mebendazole inhibits the growth and reproduction of the parasite.
In addition to antiparasitic drugs, corticosteroids may be prescribed to reduce inflammation and manage severe symptoms, such as muscle pain and swelling.
Supportive Care
Supportive care focuses on relieving symptoms and improving the patient’s overall well-being. This may include:
- Pain relievers to manage muscle pain and discomfort.
- Hydration therapy to address dehydration caused by nausea and vomiting.
- Rest and limited physical activity to allow the muscles to heal.
Preventive Measures
Preventing trichinosis involves adopting safe food handling and cooking practices. Key preventive measures include:
- Cooking meat thoroughly to an internal temperature of at least 160 degrees Fahrenheit (71 degrees Celsius).
- Freezing meat at sub-zero temperatures for an extended period to kill larvae.
- Avoiding the consumption of raw or undercooked pork, wild game, and bear meat.
- Practicing proper hygiene, such as washing hands and utensils after handling raw meat.
Public Health Initiatives
Public health organizations play a vital role in preventing trichinosis outbreaks. They educate communities about safe food practices, monitor meat production facilities, and enforce regulations to ensure the safety of meat products. Hunters and farmers are also encouraged to follow guidelines for processing and storing wild game to minimize the risk of contamination.
Living with Trichinosis
For most individuals, trichinosis resolves with appropriate treatment, and they recover fully without long-term effects. However, in severe cases, chronic muscle pain and fatigue may persist for months or even years. Regular follow-up with a healthcare provider is essential to monitor recovery and address any lingering symptoms.
When to Seek Medical Attention
Individuals who experience persistent or worsening symptoms should seek medical attention promptly. Early intervention can prevent complications and improve outcomes. Signs that warrant immediate medical care include:
- Severe muscle pain or weakness.
- Difficulty breathing or swallowing.
- High fever or signs of infection.
- Swelling of the face or throat.
Long-Term Outlook
With timely treatment and adherence to preventive measures, the prognosis for trichinosis is generally favorable. Most people recover completely, although recovery time may vary depending on the severity of the infection and the individual’s overall health.