Treacher Collins Syndrome, commonly abbreviated as TCS, is a rare genetic condition that affects the development of facial bones and tissues. This disorder leads to distinctive facial features and can cause a range of complications, from mild cosmetic differences to severe functional impairments. Understanding this condition requires an exploration of its causes, symptoms, diagnosis, and treatment options. In this article, we will delve into the intricacies of Treacher Collins Syndrome to provide a comprehensive overview.
What Causes Treacher Collins Syndrome?
The primary cause of this condition lies in genetic mutations. Specifically, it is linked to changes in certain genes responsible for the development of facial bones and tissues. These genes include TCOF1, POLR1C, and POLR1D. The mutations disrupt the normal growth and formation of structures in the face, leading to the characteristic features associated with the syndrome.
In most cases, the condition arises spontaneously due to new mutations, meaning it is not inherited from the parents. However, there are instances where it is passed down through families in an autosomal dominant pattern. This means that only one copy of the altered gene is sufficient to cause the disorder. If one parent carries the mutation, there is a 50% chance of passing it on to their offspring.
Risk Factors and Genetic Counseling
- Family History: Families with a history of the condition may benefit from genetic counseling to understand the risks of passing it to future generations.
- Advanced Parental Age: While not a definitive factor, some studies suggest that advanced parental age may slightly increase the risk of spontaneous mutations.
Genetic counseling plays a crucial role in helping families make informed decisions about family planning and understanding the likelihood of recurrence in subsequent pregnancies.
Symptoms and Physical Characteristics
The severity of symptoms can vary widely among individuals with this condition. Some may experience mild cosmetic differences, while others may face significant challenges related to breathing, hearing, and vision. Below are the most common physical characteristics associated with the syndrome:
Facial Features
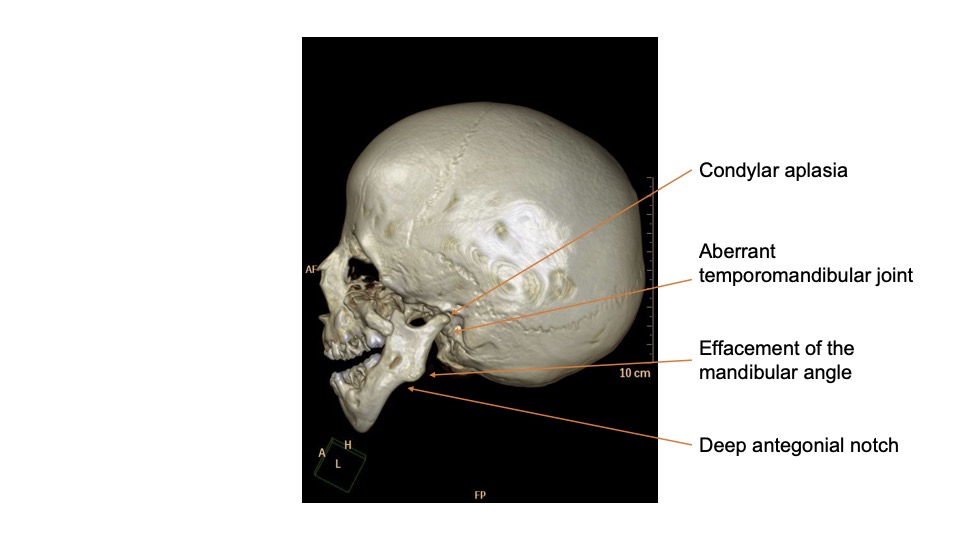
- Underdeveloped Cheekbones: The cheekbones may appear flat or sunken, giving the face a hollow appearance.
- Downward-Slanting Eyes: The outer corners of the eyes often slant downward, which is one of the hallmark features of the condition.
- Small Jaw and Chin: The lower jaw and chin may be underdeveloped, contributing to difficulties with eating and breathing.
- Cleft Palate: A split or opening in the roof of the mouth is common and can affect speech and feeding.
Hearing and Vision Issues
Individuals with this condition often experience hearing loss due to abnormalities in the ear structure. The external ear may be small, malformed, or absent altogether. Additionally, vision problems can arise from downward-slanting eyelids or the absence of lower eyelashes, which may lead to dry eyes or other complications.
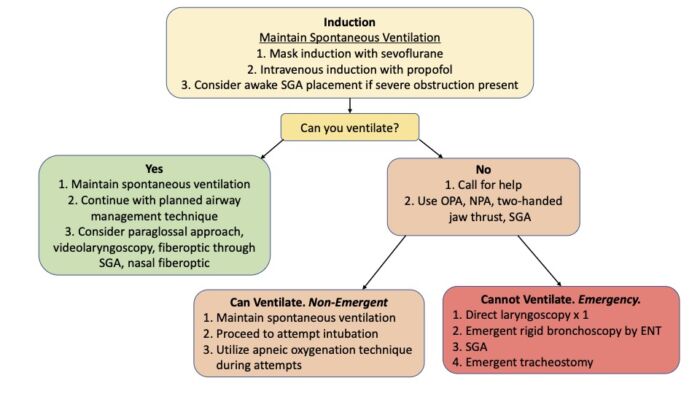
Respiratory Challenges
Underdeveloped facial bones can also impact the airway, leading to breathing difficulties. In severe cases, infants may require medical intervention to ensure proper oxygenation.
Diagnosing the Condition
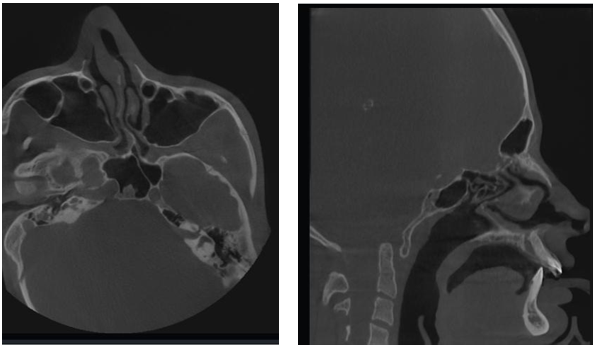
Diagnosing this syndrome typically begins with a thorough physical examination. Doctors look for the characteristic facial features and assess any functional impairments. In some cases, imaging studies such as X-rays or CT scans may be used to evaluate the extent of bone abnormalities.
Genetic Testing
Genetic testing is a key component of the diagnostic process. It involves analyzing a sample of blood or saliva to identify mutations in the relevant genes. This not only confirms the diagnosis but also helps determine whether the condition is inherited or occurred spontaneously.
Prenatal Diagnosis
In families with a known history of the condition, prenatal testing may be an option. Techniques such as amniocentesis or chorionic villus sampling can detect genetic mutations early in pregnancy. This allows parents to prepare for the potential challenges associated with the condition.
Treatment Options and Management Strategies
There is no cure for this syndrome, but various treatments can help manage the symptoms and improve quality of life. The approach to treatment is highly individualized, depending on the severity of the condition and the specific needs of the patient.
Surgical Interventions
Surgery is often necessary to address structural abnormalities. Common procedures include:
- Reconstructive Surgery: This may involve reshaping the cheekbones, jaw, or chin to improve both function and appearance.
- Ear Reconstruction: For individuals with malformed or missing ears, surgical reconstruction can enhance hearing and aesthetics.
- Cleft Palate Repair: Surgery to close the cleft palate can improve speech and feeding abilities.
Hearing Aids and Assistive Devices
Hearing loss is a common issue, and many individuals benefit from hearing aids or cochlear implants. These devices can significantly improve communication and overall quality of life.
Orthodontic Treatment
Malocclusion, or misalignment of the teeth, is frequently observed in individuals with this condition. Orthodontic interventions, such as braces or dental appliances, can help correct these issues and improve oral health.
Speech and Language Therapy
Children with this syndrome often face challenges with speech due to structural abnormalities in the mouth and throat. Speech therapy can help them develop clearer communication skills and build confidence in social interactions.
Psychological Support
Living with a visible difference can take a toll on mental health. Psychological support, including counseling and peer support groups, can help individuals and families cope with the emotional aspects of the condition.
Long-Term Outlook and Quality of Life
With appropriate medical care and support, individuals with this condition can lead fulfilling lives. Early intervention is crucial to addressing developmental delays and preventing complications. Regular follow-ups with a multidisciplinary team of specialists, including surgeons, audiologists, orthodontists, and therapists, ensure comprehensive care.
Challenges in Adulthood
While many individuals adapt well to the challenges posed by the condition, adulthood may bring additional considerations. These include ongoing dental care, potential surgeries for further refinement of facial features, and continued management of hearing and vision issues.
Advances in Research
Ongoing research into the genetic and molecular mechanisms underlying this syndrome holds promise for improved treatments in the future. Scientists are exploring gene therapies and other innovative approaches that could potentially correct the underlying mutations responsible for the condition.
Support Networks and Advocacy
Families affected by this condition often find strength in connecting with others who share similar experiences. Support networks, both online and offline, provide valuable resources and a sense of community. Advocacy organizations play a vital role in raising awareness, funding research, and promoting inclusivity for individuals with facial differences.
Building Awareness
Educating the public about this syndrome helps reduce stigma and fosters a more inclusive society. Campaigns and initiatives aimed at increasing understanding can empower individuals with the condition to live confidently and pursue their goals without fear of judgment.