Transverse Myelitis, often abbreviated as TM, is a rare neurological condition characterized by inflammation of the spinal cord. This inflammation can disrupt communication between the brain and the rest of the body, leading to a range of symptoms that vary in severity. Understanding this condition requires exploring its causes, recognizing its symptoms, diagnosing it accurately, and learning about available treatment options.
Understanding Transverse Myelitis
Transverse Myelitis is a disorder that affects the spinal cord, causing damage to the protective covering of nerve fibers, known as myelin. When the myelin is damaged, the transmission of nerve signals is impaired, leading to various physical and sensory issues. The term “transverse” refers to the fact that the inflammation occurs across the width of the spinal cord, affecting multiple levels simultaneously.
What Happens in Transverse Myelitis?
The spinal cord plays a crucial role in transmitting messages between the brain and the body. In Transverse Myelitis, the immune system mistakenly attacks the spinal cord, leading to inflammation. This inflammation can result in swelling, damage to nerve cells, and loss of myelin. As a result, individuals may experience weakness, numbness, pain, or paralysis in parts of their body below the affected area of the spinal cord.
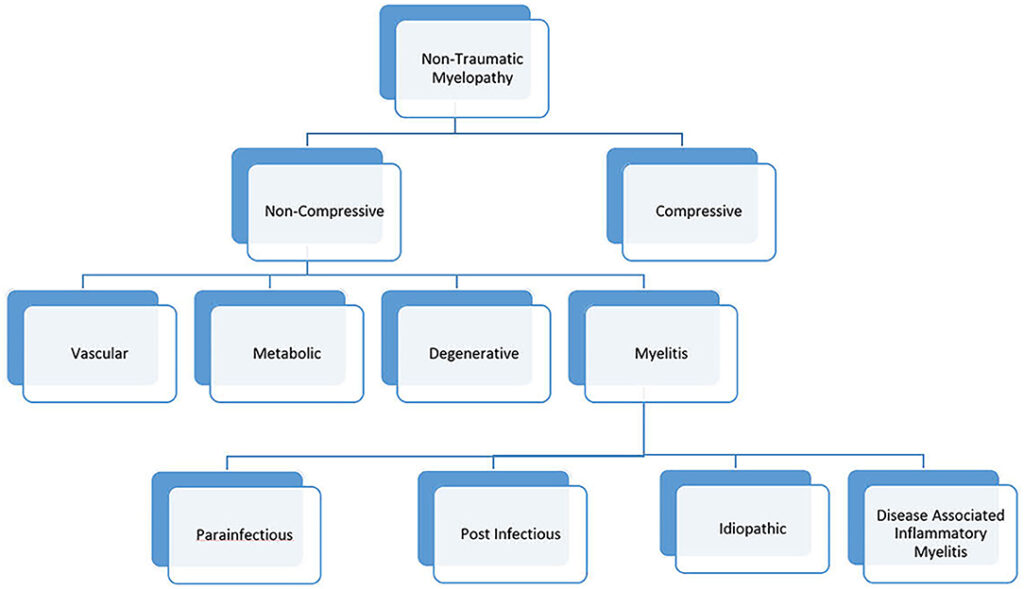
Causes of Transverse Myelitis
The exact cause of Transverse Myelitis is not always clear, but several factors have been identified as potential triggers for this condition. These include autoimmune disorders, infections, and other underlying health conditions.
Autoimmune Disorders
In some cases, Transverse Myelitis occurs when the immune system mistakenly targets the body’s own tissues. Autoimmune diseases such as multiple sclerosis and neuromyelitis optica are commonly associated with this condition. In these cases, the immune system attacks the myelin sheath, leading to inflammation and damage to the spinal cord.
Infections
Viral, bacterial, fungal, and parasitic infections can also trigger Transverse Myelitis. Common infectious agents include herpes viruses, Epstein-Barr virus, cytomegalovirus, and Lyme disease. Sometimes, the infection directly affects the spinal cord, while in other cases, the immune response to the infection leads to inflammation in the spinal cord.
Other Causes
- Vaccinations: Rarely, vaccinations have been linked to the development of Transverse Myelitis, although this is extremely uncommon.
- Vascular Disorders: Conditions that affect blood flow to the spinal cord, such as arteriovenous malformations, can lead to inflammation.
- Idiopathic Cases: In many instances, no specific cause can be identified, and the condition is classified as idiopathic.
Symptoms of Transverse Myelitis
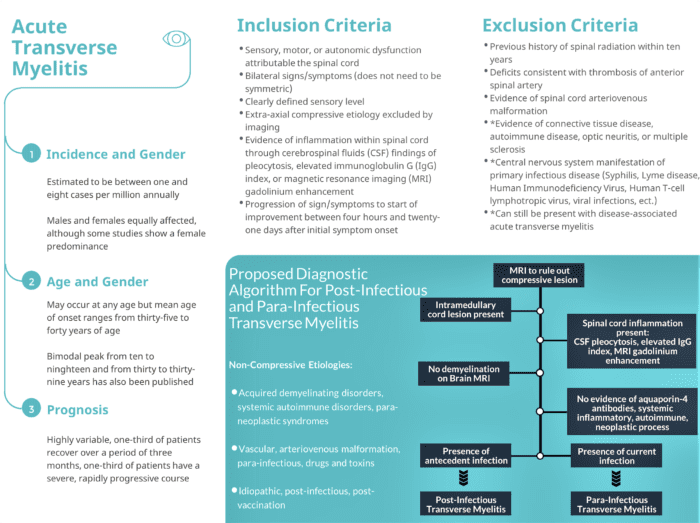
The symptoms of Transverse Myelitis can vary widely depending on the location and severity of the inflammation. They often develop rapidly over hours or days and can include sensory, motor, and autonomic dysfunction.
Sensory Symptoms
Individuals with Transverse Myelitis may experience abnormal sensations such as burning, tingling, numbness, or coldness in their limbs or torso. Some people describe these sensations as a tight band around their chest or abdomen. Pain is also common, often described as sharp, shooting, or aching, and it may worsen with movement.
Motor Symptoms
Weakness in the arms or legs is a hallmark symptom of Transverse Myelitis. In severe cases, this weakness can progress to partial or complete paralysis. Muscle spasms, stiffness, and difficulty coordinating movements are also common. Over time, muscle atrophy may occur due to disuse.
Autonomic Symptoms
Autonomic dysfunction refers to problems with involuntary bodily functions. People with Transverse Myelitis may experience bladder and bowel dysfunction, including incontinence or difficulty urinating. Other symptoms include sexual dysfunction, abnormal blood pressure, and changes in body temperature regulation.
Diagnosis of Transverse Myelitis
Diagnosing Transverse Myelitis involves a combination of clinical evaluation, imaging studies, and laboratory tests. Since the symptoms of this condition overlap with those of other neurological disorders, a thorough diagnostic process is essential to rule out alternative causes.
Clinical Evaluation
A healthcare provider will begin by taking a detailed medical history and conducting a physical examination. They will assess the patient’s reflexes, muscle strength, coordination, and sensory responses. Any recent illnesses, vaccinations, or underlying health conditions will also be noted.
Magnetic Resonance Imaging
Magnetic resonance imaging is a key tool in diagnosing Transverse Myelitis. It provides detailed images of the spinal cord, allowing doctors to identify areas of inflammation, swelling, or lesions. In some cases, contrast agents may be used to enhance the visibility of abnormalities.
Laboratory Tests
Blood tests and cerebrospinal fluid analysis are often performed to check for signs of infection, inflammation, or autoimmune activity. Elevated levels of certain proteins or white blood cells in the cerebrospinal fluid can indicate an inflammatory process in the spinal cord.
Additional Tests
In some cases, additional tests such as electromyography or nerve conduction studies may be conducted to evaluate nerve function. These tests help differentiate Transverse Myelitis from other conditions like Guillain-Barre syndrome or amyotrophic lateral sclerosis.
Treatment of Transverse Myelitis
While there is no cure for Transverse Myelitis, early and aggressive treatment can help reduce inflammation, manage symptoms, and improve long-term outcomes. Treatment typically involves medications, rehabilitation therapies, and supportive care.
Medications
Several types of medications are used to treat Transverse Myelitis:
- Corticosteroids: High-dose intravenous corticosteroids, such as methylprednisolone, are often administered to reduce inflammation and suppress the immune response.
- Plasma Exchange Therapy: If corticosteroids are ineffective, plasma exchange therapy may be recommended. This procedure removes harmful antibodies and inflammatory substances from the blood.
- Immunosuppressants: For individuals with underlying autoimmune disorders, medications that suppress the immune system may be prescribed to prevent further attacks.
Rehabilitation Therapies
Physical therapy, occupational therapy, and speech therapy play a vital role in recovery. These therapies aim to restore mobility, improve strength and coordination, and help patients regain independence in daily activities. Assistive devices such as braces, walkers, or wheelchairs may also be recommended based on the individual’s needs.
Supportive Care
Managing symptoms and complications is an important aspect of treatment. This includes addressing pain with medications, managing bladder and bowel dysfunction, and providing psychological support to cope with the emotional impact of the condition. Regular follow-up appointments are necessary to monitor progress and adjust treatment plans as needed.
Experimental Treatments
Researchers are continually exploring new treatments for Transverse Myelitis. Clinical trials are underway to investigate the effectiveness of stem cell therapy, monoclonal antibodies, and other innovative approaches. Patients interested in participating in these trials should consult their healthcare providers for more information.
Living with Transverse Myelitis
Living with Transverse Myelitis can be challenging, but many individuals achieve significant improvement with proper treatment and support. Education, advocacy, and connecting with others who have the condition can provide valuable resources and encouragement. Support groups and organizations dedicated to Transverse Myelitis offer opportunities to share experiences and learn from others facing similar challenges.