Toxic Shock Syndrome, often abbreviated as TSS, is a rare but potentially life-threatening condition caused by bacterial toxins. It gained significant attention in the 1980s due to its association with tampon use, but it can affect anyone regardless of age or gender. This article delves into the causes, symptoms, risk factors, diagnosis, treatment, and prevention of this serious medical condition.
Understanding Toxic Shock Syndrome
Toxic Shock Syndrome is a severe illness triggered by toxins produced by certain strains of bacteria, most commonly Staphylococcus aureus and Streptococcus pyogenes. These bacteria are typically found on the skin or in the nose and throat of healthy individuals. However, under specific conditions, they can release toxins that enter the bloodstream, leading to widespread inflammation and organ dysfunction.
How Toxic Shock Syndrome Develops
The development of Toxic Shock Syndrome involves a complex interaction between bacterial toxins and the immune system. When these toxins enter the bloodstream, they can bind to immune cells and trigger an exaggerated inflammatory response. This response can cause damage to multiple organs, including the kidneys, liver, and lungs, making the condition particularly dangerous if not treated promptly.
Symptoms of Toxic Shock Syndrome
The symptoms of Toxic Shock Syndrome can appear suddenly and progress rapidly. Recognizing these symptoms early is crucial for timely medical intervention. Below are the common signs associated with this condition:
- High fever, often exceeding 102 degrees Fahrenheit
- Low blood pressure, which may lead to dizziness or fainting
- A sunburn-like rash, particularly on the palms and soles
- Vomiting or diarrhea
- Muscle aches and weakness
- Confusion or disorientation
- Redness of the eyes, mouth, and throat
It is important to note that not all individuals will experience every symptom, and the severity can vary widely. In some cases, the condition may mimic other illnesses, making diagnosis challenging.
Causes and Risk Factors
Bacterial Origins
Toxic Shock Syndrome is primarily caused by toxins produced by two types of bacteria: Staphylococcus aureus and Streptococcus pyogenes. While both bacteria are commonly found in the human body, they usually do not cause harm unless specific conditions allow them to multiply and release toxins. For instance, Staphylococcus aureus is often linked to tampon use, while Streptococcus pyogenes is more frequently associated with skin infections or wounds.
Risk Factors
Certain factors can increase the likelihood of developing Toxic Shock Syndrome. These include:
- Recent surgery or childbirth
- Use of highly absorbent tampons during menstruation
- Skin injuries, such as cuts, burns, or surgical wounds
- Weakened immune system due to conditions like diabetes or cancer
- Recent use of barrier contraceptives, such as diaphragms or sponges
While women of reproductive age are at higher risk due to tampon use, men and children can also develop this condition, especially if they have open wounds or underlying health issues.
Diagnosis of Toxic Shock Syndrome
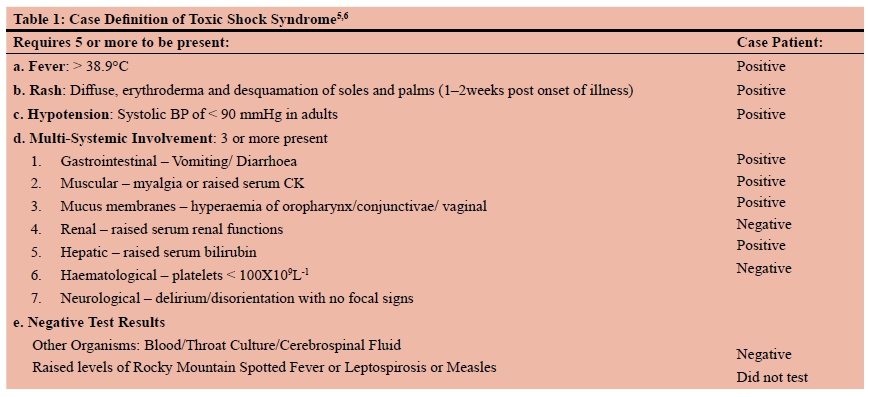
Diagnosing Toxic Shock Syndrome requires a thorough evaluation by a healthcare professional. There is no single test to confirm the condition, so doctors rely on a combination of clinical findings, laboratory tests, and patient history to make an accurate diagnosis.
Clinical Assessment
During the initial assessment, the doctor will review the patient’s symptoms and medical history. They may ask about recent tampon use, surgeries, or any skin injuries. The presence of a characteristic rash and low blood pressure can raise suspicion of Toxic Shock Syndrome.
Laboratory Tests
Several laboratory tests can help support the diagnosis:
- Blood tests to check for elevated white blood cell counts and markers of inflammation
- Kidney and liver function tests to assess organ damage
- Cultures of blood, urine, or wound samples to identify the presence of toxin-producing bacteria
In some cases, imaging studies such as X-rays or CT scans may be performed to evaluate complications like fluid buildup in the lungs or internal infections.
Treatment Options
Treatment for Toxic Shock Syndrome must begin immediately to prevent complications and improve outcomes. The approach typically involves hospitalization and a combination of interventions aimed at addressing the infection and supporting affected organs.
Antibiotics
Since Toxic Shock Syndrome is caused by bacterial toxins, antibiotics play a critical role in treatment. Broad-spectrum antibiotics are often administered intravenously to target the bacteria responsible for the infection. The choice of antibiotics may be adjusted based on culture results and the patient’s response to treatment.
Fluid Replacement
Low blood pressure is a hallmark of Toxic Shock Syndrome and can lead to shock if not managed promptly. Intravenous fluids are given to stabilize blood pressure and ensure adequate circulation to vital organs. In severe cases, medications to raise blood pressure may also be required.
Supportive Care
Patients with Toxic Shock Syndrome may require additional supportive measures, depending on the severity of their condition. These can include:
- Oxygen therapy or mechanical ventilation for respiratory distress
- Dialysis for kidney failure
- Pain management and medications to reduce inflammation
In cases where the infection originates from a tampon or foreign object, prompt removal is essential to stop the source of toxin production.
Prevention Strategies
While Toxic Shock Syndrome cannot always be prevented, certain measures can significantly reduce the risk of developing this condition. Awareness and education are key components of prevention, especially for individuals who use tampons or have underlying health conditions.
Safe Tampon Use
For women who use tampons, adopting safe practices can minimize the risk of Toxic Shock Syndrome:
- Use the lowest absorbency tampon necessary for your flow
- Change tampons every four to eight hours
- Alternate between tampons and sanitary pads during menstruation
- Avoid using tampons overnight
It is also advisable to wash hands thoroughly before and after inserting or removing tampons to reduce the risk of introducing bacteria.
Proper Wound Care
Individuals with skin injuries or surgical wounds should take steps to prevent infection:
- Keep wounds clean and covered with sterile dressings
- Wash hands regularly, especially before touching wounds
- Seek medical attention for signs of infection, such as redness, swelling, or pus
Early treatment of infections can prevent the progression to Toxic Shock Syndrome.
General Hygiene Practices
Maintaining good hygiene is another effective way to reduce the risk of Toxic Shock Syndrome:
- Regularly wash hands with soap and water
- Avoid sharing personal items like razors or towels
- Stay up-to-date with vaccinations to strengthen the immune system
For individuals with weakened immune systems, additional precautions may be necessary to prevent infections.
Complications of Toxic Shock Syndrome
If left untreated, Toxic Shock Syndrome can lead to severe complications that affect multiple organs. These complications may include:
- Kidney failure requiring dialysis
- Liver damage or failure
- Respiratory distress or acute respiratory failure
- Seizures or neurological damage
- Shock and multi-organ failure
Even with prompt treatment, some individuals may experience long-term effects, such as chronic fatigue or muscle weakness. Regular follow-up care is essential to monitor recovery and address any lingering issues.
Public Awareness and Education
Raising awareness about Toxic Shock Syndrome is critical to ensuring early recognition and treatment. Public health campaigns, educational programs, and clear labeling on tampon packaging can empower individuals to make informed decisions about their health. Healthcare providers also play a vital role in educating patients about the risks and prevention strategies associated with this condition.
By fostering a better understanding of Toxic Shock Syndrome, we can reduce its incidence and improve outcomes for those affected by this serious illness.





