Thyroid cancer, often abbreviated as TC, is a type of cancer that originates in the thyroid gland. This small, butterfly-shaped gland located at the base of the neck plays a crucial role in regulating metabolism, energy production, and overall hormonal balance. While thyroid cancer is relatively rare compared to other types of cancer, its incidence has been increasing over the years. Understanding its types, recognizing its symptoms, undergoing proper diagnosis, and exploring available treatments are essential steps in managing this condition effectively.
Types of Thyroid Cancer
Thyroid cancer can be classified into several distinct types based on the specific cells within the thyroid gland where the cancer originates. Each type has unique characteristics, growth patterns, and treatment approaches.
Papillary Thyroid Cancer
Papillary thyroid cancer is the most common type, accounting for approximately eighty percent of all cases. It typically grows slowly and often affects only one lobe of the thyroid gland. This type of cancer tends to spread to nearby lymph nodes but is usually highly treatable, especially when detected early. People diagnosed with papillary thyroid cancer often have an excellent prognosis.
Follicular Thyroid Cancer
Follicular thyroid cancer makes up about ten to fifteen percent of thyroid cancer cases. It arises from the follicular cells, which are responsible for producing thyroid hormones. Unlike papillary thyroid cancer, follicular thyroid cancer is less likely to spread to the lymph nodes but may metastasize to distant organs such as the lungs or bones. Early detection and treatment are critical for improving outcomes.
Medullary Thyroid Cancer
Medullary thyroid cancer originates in the C cells of the thyroid gland, which produce calcitonin, a hormone involved in calcium regulation. This type accounts for about four percent of thyroid cancer cases. Medullary thyroid cancer can occur sporadically or as part of an inherited syndrome known as multiple endocrine neoplasia. It tends to be more aggressive than papillary or follicular thyroid cancer and requires careful monitoring and management.
Anaplastic Thyroid Cancer
Anaplastic thyroid cancer is a rare and aggressive form of thyroid cancer, representing less than two percent of cases. It grows rapidly and is often difficult to treat because it does not respond well to conventional therapies. Anaplastic thyroid cancer is more common in older adults and is associated with a poorer prognosis compared to other types.
Thyroid Lymphoma
Thyroid lymphoma is an extremely rare type of cancer that begins in the immune cells within the thyroid gland. It is more commonly seen in individuals with pre-existing thyroid conditions such as Hashimoto’s thyroiditis. Treatment typically involves chemotherapy and radiation therapy, depending on the stage and extent of the disease.
Symptoms of Thyroid Cancer
Recognizing the symptoms of thyroid cancer is vital for early detection and timely intervention. However, it is important to note that many of these symptoms can also be caused by benign thyroid conditions or other unrelated health issues. Some of the most common signs include:
- A lump or swelling in the neck, often near the Adam’s apple
- Hoarseness or changes in voice that persist for an extended period
- Difficulty swallowing or a sensation of something stuck in the throat
- Pain in the neck or throat that may radiate to the ears
- Swollen lymph nodes in the neck
In some cases, thyroid cancer may not cause any noticeable symptoms until it has progressed to an advanced stage. Regular check-ups and screenings can help identify potential issues before they become severe.
Diagnosis of Thyroid Cancer
Diagnosing thyroid cancer involves a combination of physical examinations, imaging tests, and laboratory analyses. The process typically begins with a thorough evaluation by a healthcare provider, who will assess the patient’s medical history and perform a physical examination to check for abnormalities in the neck area.
Physical Examination
During a physical examination, the doctor will carefully feel the neck for any lumps, nodules, or irregularities in the thyroid gland. They may also ask questions about symptoms such as hoarseness, difficulty swallowing, or persistent pain in the neck.
Ultrasound Imaging
An ultrasound is a non-invasive imaging test that uses sound waves to create detailed pictures of the thyroid gland. This test helps identify the size, shape, and location of any nodules or masses. Ultrasound can also determine whether a nodule is solid or filled with fluid, which provides valuable information about its likelihood of being cancerous.
Fine-Needle Aspiration Biopsy
If a suspicious nodule is detected, a fine-needle aspiration biopsy may be performed. During this procedure, a thin needle is inserted into the nodule to extract a small sample of cells. These cells are then examined under a microscope to determine whether they are cancerous. Fine-needle aspiration biopsy is considered the gold standard for diagnosing thyroid cancer.
Blood Tests
Blood tests are used to measure levels of thyroid hormones and other substances, such as calcitonin and thyroglobulin, which can provide additional clues about the presence of thyroid cancer. Elevated levels of certain markers may indicate the need for further investigation.
Imaging Tests
In some cases, additional imaging tests such as computed tomography scans or magnetic resonance imaging may be required to assess the extent of the cancer and determine whether it has spread to other parts of the body. These tests help guide treatment decisions and develop a comprehensive care plan.
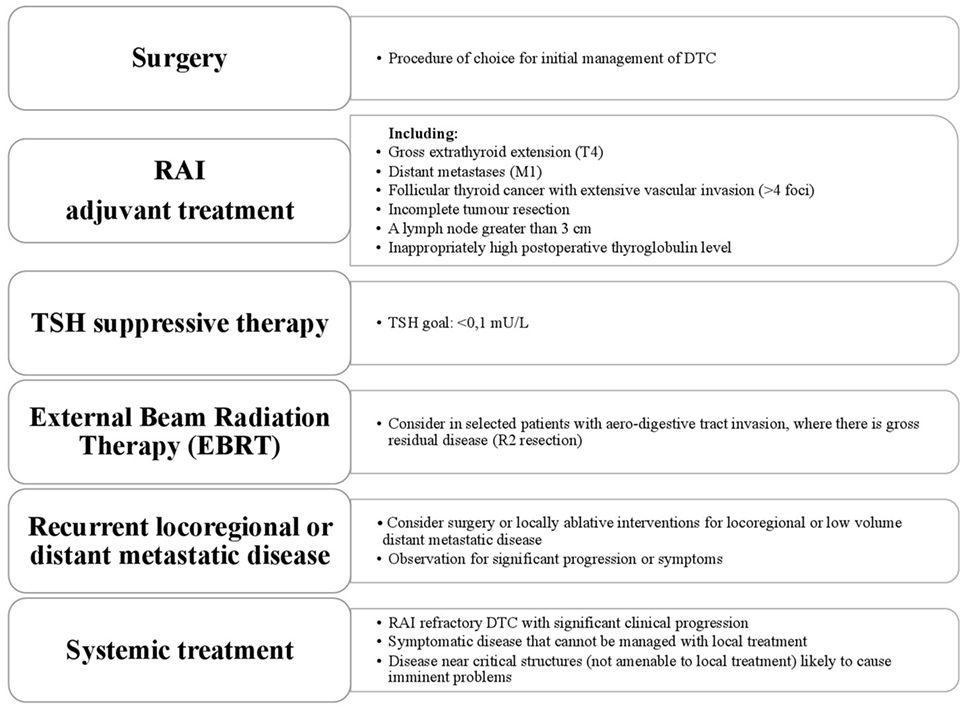
Treatments for Thyroid Cancer
The treatment approach for thyroid cancer depends on several factors, including the type and stage of the cancer, the patient’s age and overall health, and their personal preferences. Below are some of the most common treatment options:
Surgery
Surgery is the primary treatment for most types of thyroid cancer. The goal of surgery is to remove the cancerous tissue while preserving as much of the healthy thyroid gland as possible. There are two main types of surgical procedures:
- Thyroidectomy: This involves the complete removal of the thyroid gland. After a thyroidectomy, patients will need to take synthetic thyroid hormone replacement medication for the rest of their lives to maintain normal metabolic function.
- Lobectomy: In this procedure, only the affected lobe of the thyroid gland is removed. Lobectomy is typically performed for small, low-risk cancers and allows the remaining portion of the thyroid to continue functioning normally.
Radiation Therapy
Radiation therapy uses high-energy beams to target and destroy cancer cells. For thyroid cancer, a specialized form of radiation therapy called radioactive iodine therapy is often used. Radioactive iodine is absorbed by thyroid cells, including cancerous ones, and helps eliminate residual thyroid tissue or metastatic disease after surgery.
Hormone Therapy
Hormone therapy involves taking synthetic thyroid hormones to replace those no longer produced by the thyroid gland after surgery. In addition to restoring normal hormone levels, hormone therapy can also suppress the production of thyroid-stimulating hormone, which may reduce the risk of cancer recurrence.
Targeted Drug Therapy
Targeted drug therapy is used to treat advanced or metastatic thyroid cancer that does not respond to traditional treatments. These medications work by targeting specific molecules or pathways involved in cancer cell growth and survival. Examples include tyrosine kinase inhibitors, which block signals that promote tumor development.
Chemotherapy
Chemotherapy is rarely used for thyroid cancer but may be considered for aggressive or refractory cases, such as anaplastic thyroid cancer. Chemotherapy drugs are administered intravenously or orally and work by killing rapidly dividing cancer cells throughout the body.
External Beam Radiation Therapy
External beam radiation therapy delivers focused radiation to specific areas of the body affected by cancer. This treatment is typically reserved for cases where the cancer has spread to nearby structures or cannot be completely removed through surgery.
Clinical Trials
For patients with advanced or recurrent thyroid cancer, participation in clinical trials may offer access to innovative treatments and therapies that are not yet widely available. Clinical trials play a crucial role in advancing our understanding of thyroid cancer and improving outcomes for future patients.
Living with Thyroid Cancer
Managing thyroid cancer requires a multidisciplinary approach involving endocrinologists, surgeons, oncologists, and other healthcare professionals. Patients are encouraged to stay informed about their condition, actively participate in treatment decisions, and seek support from family, friends, and support groups. Coping strategies such as mindfulness, exercise, and counseling can also help improve quality of life during and after treatment.