Vitamin B1, also known as thiamine, is an essential nutrient that plays a critical role in maintaining overall health. A deficiency in this vital nutrient, often abbreviated as TD, can lead to serious health complications if left untreated. In this article, we will explore the causes, symptoms, diagnosis, and treatment of thiamine deficiency in detail.
What is Thiamine?
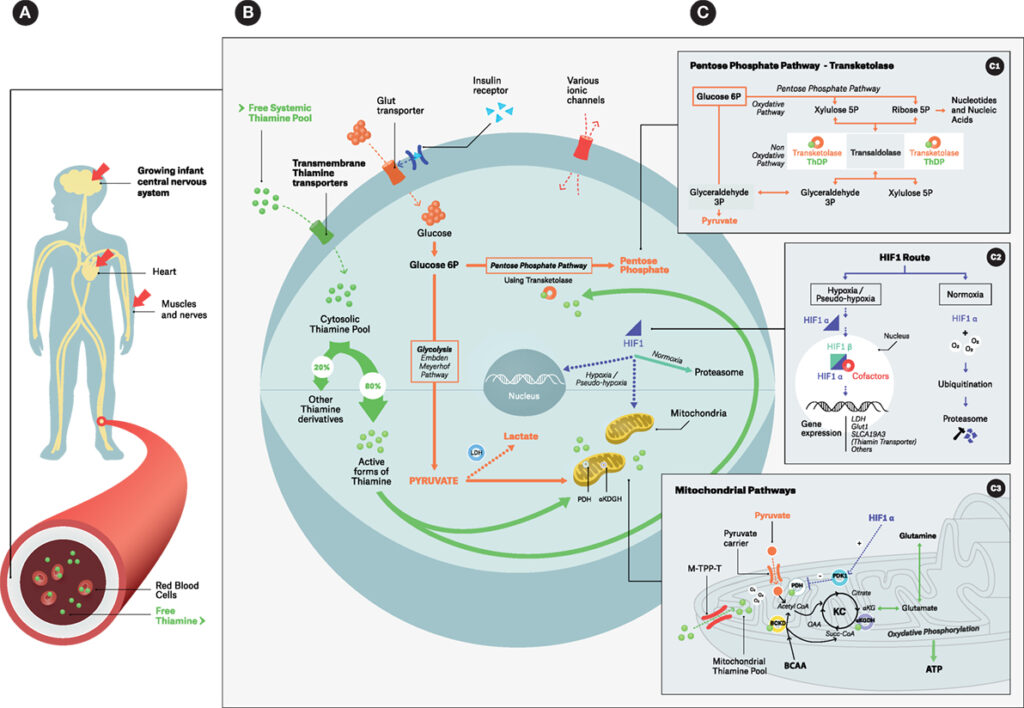
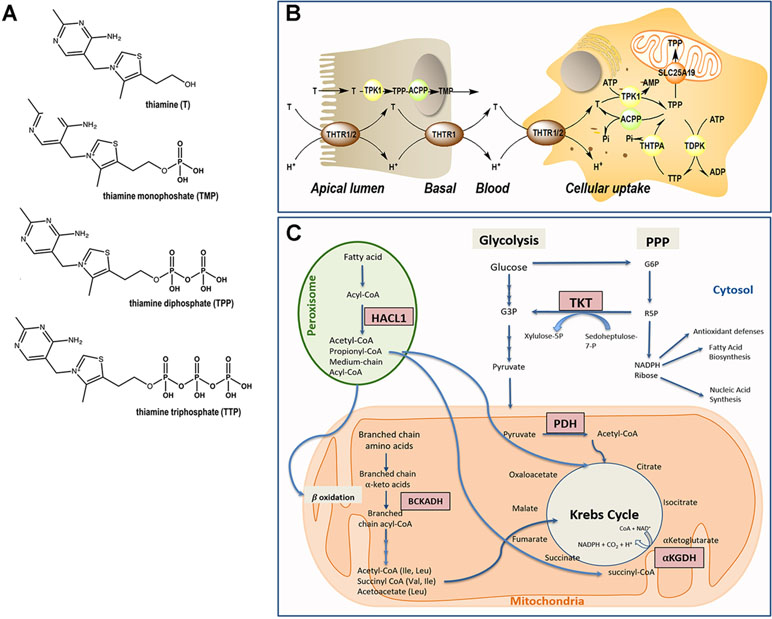
Thiamine is one of the eight B vitamins and is crucial for converting food into energy. It helps the body metabolize carbohydrates and supports the proper functioning of the nervous system, muscles, and heart. Without sufficient thiamine, the body cannot produce enough energy to sustain basic cellular functions, leading to various health issues.
Causes of Thiamine Deficiency
There are several reasons why someone might develop a deficiency in thiamine. Understanding these causes is key to prevention and early intervention.
Poor Dietary Intake
- A diet lacking in foods rich in thiamine, such as whole grains, legumes, nuts, and lean meats, can lead to a deficiency.
- People who consume highly processed foods or follow restrictive diets may not get enough thiamine from their meals.
Alcoholism
Chronic alcohol consumption is one of the most common causes of thiamine deficiency. Alcohol interferes with the absorption of thiamine in the digestive tract and reduces its storage in the liver. Additionally, individuals with alcohol use disorder often have poor dietary habits, further exacerbating the problem.
Gastrointestinal Disorders
- Conditions like Crohn’s disease, celiac disease, and ulcerative colitis can impair the absorption of nutrients, including thiamine.
- Bariatric surgery or other procedures that alter the digestive system can also reduce the body’s ability to absorb thiamine.
Prolonged Use of Diuretics
Certain medications, such as diuretics, can increase the excretion of thiamine through urine, leading to a deficiency over time. This is particularly concerning for individuals with heart failure or kidney problems who rely on these medications.
Increased Physiological Demand
- Pregnancy and breastfeeding increase the body’s need for thiamine.
- Intense physical activity or illnesses that cause fever can also raise the demand for this nutrient.
Symptoms of Thiamine Deficiency
The symptoms of thiamine deficiency can vary depending on the severity and duration of the condition. Early signs are often subtle but can progress to more severe complications if left untreated.
Mild Symptoms
- Fatigue and weakness
- Irritability and confusion
- Loss of appetite
- Weight loss
Severe Symptoms
- Beriberi: This condition affects the cardiovascular and nervous systems. Wet beriberi leads to heart failure and edema, while dry beriberi causes nerve damage and muscle weakness.
- Wernicke-Korsakoff Syndrome: Often seen in people with chronic alcoholism, this syndrome includes Wernicke’s encephalopathy (confusion, difficulty walking, and eye movement problems) and Korsakoff psychosis (memory loss and hallucinations).
- Neuropathy: Nerve damage resulting in tingling, numbness, or burning sensations in the extremities.
Diagnosis of Thiamine Deficiency
Diagnosing thiamine deficiency can be challenging because its symptoms overlap with those of other conditions. However, healthcare providers use a combination of clinical evaluation, medical history, and laboratory tests to confirm the diagnosis.
Clinical Evaluation
A doctor will assess the patient’s symptoms, dietary habits, and lifestyle factors. They may ask about alcohol consumption, gastrointestinal issues, or recent surgeries that could contribute to the deficiency.
Laboratory Tests
- Blood tests to measure thiamine levels directly or assess related markers such as erythrocyte transketolase activity.
- Urinary tests to evaluate thiamine excretion.
Imaging and Neurological Exams
In cases where neurological symptoms are present, imaging studies like MRI scans may be used to rule out other causes. Neurological exams help identify specific deficits associated with thiamine deficiency.
Treatment of Thiamine Deficiency
The treatment for thiamine deficiency focuses on replenishing thiamine levels and addressing any underlying causes. Early intervention is crucial to prevent long-term complications.
Thiamine Supplementation
Oral supplements are typically prescribed for mild deficiencies. For more severe cases, intravenous or intramuscular injections of thiamine may be necessary to quickly restore levels. The dosage and duration depend on the individual’s condition and response to treatment.
Dietary Changes
Incorporating thiamine-rich foods into the diet is essential for long-term recovery. These include:
- Whole grains (brown rice, oats, quinoa)
- Legumes (lentils, beans, peas)
- Nuts and seeds (sunflower seeds, macadamia nuts)
- Lean meats (pork, beef)
- Fruits and vegetables (oranges, spinach, asparagus)
Treating Underlying Conditions
If the deficiency is caused by a gastrointestinal disorder, managing that condition is vital. Similarly, individuals with alcohol use disorder may require counseling, rehabilitation, or medication to address their addiction.
Monitoring and Follow-Up
Regular follow-up appointments are necessary to monitor progress and adjust treatment as needed. Blood tests may be repeated to ensure thiamine levels return to normal.
Prevention of Thiamine Deficiency
Preventing thiamine deficiency involves adopting healthy dietary habits and addressing risk factors early. Some preventive measures include:
- Eating a balanced diet rich in whole foods.
- Avoiding excessive alcohol consumption.
- Seeking medical advice before starting restrictive diets or undergoing weight-loss surgeries.
- Taking multivitamin supplements if recommended by a healthcare provider.
Special Considerations
Certain populations are at higher risk of developing thiamine deficiency and require special attention:
- Pregnant and breastfeeding women
- Older adults, especially those with limited mobility or poor nutrition
- Individuals with chronic illnesses or malabsorption disorders
Healthcare providers should screen these groups regularly and provide appropriate guidance to prevent deficiencies.