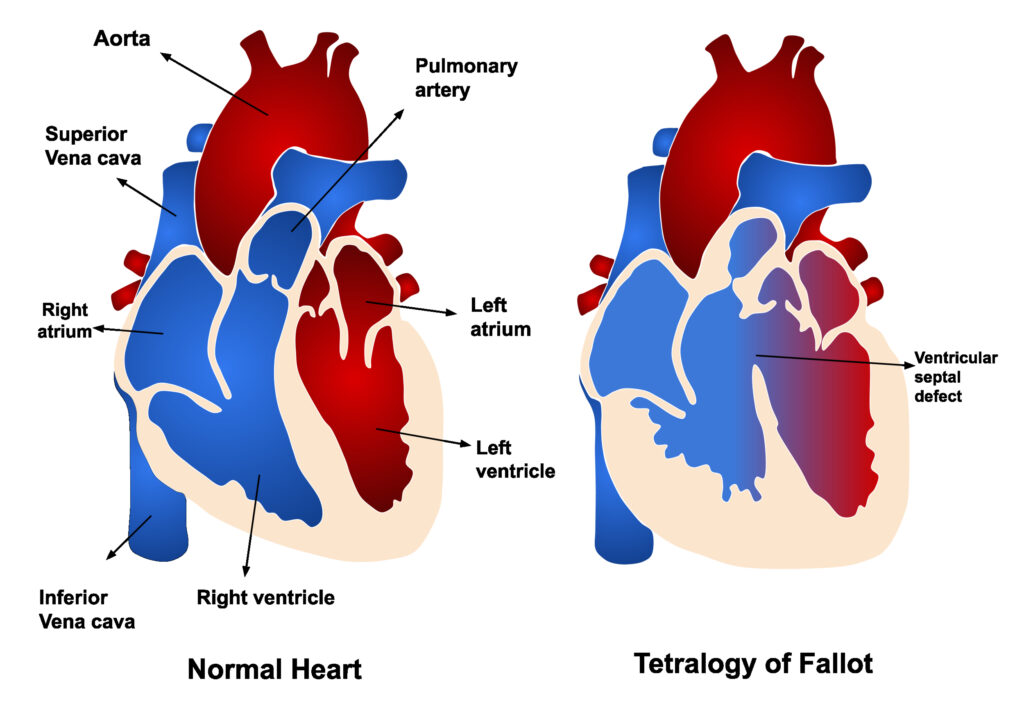
Tetralogy of Fallot, commonly abbreviated as TOF, is a congenital heart defect that affects the structure of the heart and how blood flows through it. This condition involves four specific abnormalities in the heart’s anatomy, which together cause oxygen-poor blood to mix with oxygen-rich blood, leading to inadequate oxygen supply throughout the body. In this article, we will explore the overview, causes, symptoms, and treatments associated with this complex condition.
Overview of Tetralogy of Fallot
Tetralogy of Fallot is one of the most common congenital heart defects diagnosed in newborns. It occurs when there are structural problems within the heart that develop during fetal growth. These abnormalities affect how blood circulates, causing insufficient oxygen levels in the bloodstream. As a result, individuals with this condition may experience symptoms such as cyanosis, or bluish discoloration of the skin, due to low oxygen levels.
The condition is named after the French physician Étienne-Louis Arthur Fallot, who first described it in 1888. Although advancements in medical science have improved outcomes for affected individuals, early diagnosis and treatment remain critical for managing the condition effectively.
Four Defects in Tetralogy of Fallot
- Ventricular Septal Defect: A hole exists between the two lower chambers of the heart, allowing oxygen-poor and oxygen-rich blood to mix.
- Pulmonary Stenosis: The pulmonary valve, which controls blood flow from the heart to the lungs, is narrowed, restricting the amount of blood reaching the lungs for oxygenation.
- Right Ventricular Hypertrophy: The muscle of the right ventricle becomes thickened due to the increased effort required to pump blood through the narrowed pulmonary valve.
- Overriding Aorta: The aorta, the main artery carrying oxygenated blood to the body, is positioned over the ventricular septal defect, allowing it to receive both oxygen-poor and oxygen-rich blood.
Causes of Tetralogy of Fallot
The exact cause of Tetralogy of Fallot is not fully understood, but researchers believe it results from a combination of genetic and environmental factors. Below are some potential contributors to the development of this condition:
Genetic Factors
Certain genetic syndromes, such as Down syndrome and DiGeorge syndrome, are associated with an increased risk of developing Tetralogy of Fallot. Additionally, if a parent or sibling has a congenital heart defect, the likelihood of the condition occurring in other family members may be higher.
Environmental Influences
Exposure to certain environmental factors during pregnancy can increase the risk of congenital heart defects. These include:
- Maternal infections, such as rubella, during the first trimester of pregnancy.
- Use of alcohol or tobacco during pregnancy.
- Poorly controlled diabetes in the mother.
- Exposure to certain medications or chemicals.
Unknown Factors
In many cases, no clear cause can be identified. Researchers continue to study the condition to better understand its origins and improve prevention strategies.
Symptoms of Tetralogy of Fallot
The symptoms of Tetralogy of Fallot vary depending on the severity of the defects and the age of the individual. In infants and young children, the following signs are commonly observed:
Cyanosis
Cyanosis is one of the hallmark symptoms of Tetralogy of Fallot. It manifests as a bluish tint to the skin, lips, and nails due to low oxygen levels in the blood. This symptom often becomes more noticeable during physical activity or crying, as the body demands more oxygen.
Difficulty Breathing
Infants with this condition may experience rapid breathing or difficulty breathing, especially during feeding. This can lead to poor weight gain and fatigue.
Fainting or Loss of Consciousness
Some children may experience episodes of fainting or loss of consciousness, known as “tet spells.” These occur when oxygen levels drop suddenly, often triggered by crying, physical exertion, or stress.
Fatigue
Due to the reduced oxygen supply, children with Tetralogy of Fallot may tire easily during activities that require physical effort.
Heart Murmur
A heart murmur, or an abnormal sound heard during a heartbeat, is often detected during a routine physical examination. While not always a sign of Tetralogy of Fallot, it can prompt further investigation into the heart’s structure and function.
Diagnosis of Tetralogy of Fallot
Early diagnosis is crucial for managing Tetralogy of Fallot effectively. Healthcare providers use a combination of methods to identify the condition:
Physical Examination
A healthcare provider may notice signs such as cyanosis, a heart murmur, or poor growth during a physical exam. These findings can raise suspicion of a congenital heart defect.
Diagnostic Tests
Several tests are used to confirm the presence of Tetralogy of Fallot:
- Echocardiogram: This ultrasound of the heart provides detailed images of its structure and function, helping to identify the four defects associated with the condition.
- Chest X-ray: An X-ray of the chest can reveal an enlarged heart or other abnormalities in the heart and lungs.
- Electrocardiogram: This test measures the electrical activity of the heart and can detect irregularities in heart rhythm or thickening of the heart muscle.
- Cardiac Catheterization: In some cases, a thin tube is inserted into a blood vessel and guided to the heart to measure pressures and oxygen levels within the heart chambers.
Treatment Options for Tetralogy of Fallot
Treatment for Tetralogy of Fallot focuses on improving blood flow and oxygenation. The approach depends on the severity of the condition and the age of the patient. In most cases, surgical intervention is necessary to correct the structural abnormalities.
Medications
While medications cannot cure Tetralogy of Fallot, they can help manage symptoms and stabilize the patient before surgery. Common medications include:
- Prostaglandins: These drugs help keep the ductus arteriosus open in newborns, allowing blood to flow to the lungs until surgery can be performed.
- Beta-blockers: These may be prescribed to reduce the frequency of tet spells by slowing the heart rate.
Surgical Interventions
Surgery is the primary treatment for Tetralogy of Fallot. There are two main types of procedures:
Temporary Shunt Placement
In some cases, a temporary shunt may be placed to improve blood flow to the lungs. This procedure is typically performed in infants who are too small or unstable for complete repair.
Complete Surgical Repair
Complete repair is the definitive treatment for Tetralogy of Fallot. During this procedure, surgeons address all four defects:
- The ventricular septal defect is closed using a patch.
- The pulmonary valve is widened to relieve stenosis.
- The position of the aorta is corrected to ensure proper blood flow.
This surgery is usually performed within the first year of life, although the timing may vary based on the child’s condition.
Long-Term Monitoring
Even after successful surgery, individuals with Tetralogy of Fallot require lifelong monitoring by a cardiologist. This is because complications such as arrhythmias, pulmonary valve regurgitation, or residual defects may arise later in life. Regular follow-up appointments, imaging tests, and electrocardiograms are essential for maintaining heart health.
Living with Tetralogy of Fallot
With advances in medical care, many individuals with Tetralogy of Fallot can lead active and fulfilling lives. However, certain lifestyle adjustments may be necessary to accommodate the condition:
Exercise and Physical Activity
While moderate exercise is generally safe, individuals should consult their healthcare provider to determine appropriate activities. High-intensity sports or activities that strain the heart may need to be avoided.
Preventing Infections
Individuals with Tetralogy of Fallot are at an increased risk of infections, particularly endocarditis, an infection of the heart lining. Antibiotics may be prescribed before certain dental or surgical procedures to reduce this risk.
Emotional and Psychological Support
Living with a chronic condition can be challenging, both for the individual and their family. Counseling, support groups, and educational resources can provide valuable assistance in coping with the emotional aspects of the condition.