Testicular cancer, often abbreviated as TC, is a relatively rare form of cancer that primarily affects younger men, typically between the ages of fifteen and thirty-five. Despite its rarity, it is one of the most treatable forms of cancer when detected early. Understanding its types, causes, symptoms, and available treatments can help individuals recognize warning signs and seek timely medical attention. This article delves into these aspects to provide a comprehensive overview of testicular cancer.
Understanding Testicular Cancer
Testicular cancer originates in the testicles, which are part of the male reproductive system. The testicles are responsible for producing sperm and testosterone, making them vital for fertility and hormonal balance. When abnormal cells begin to grow uncontrollably in the testicles, they can form tumors that may spread to other parts of the body if left untreated.
Types of Testicular Cancer
There are several types of testicular cancer, each classified based on the type of cells involved. These include:
- Germ Cell Tumors: These account for the majority of cases and originate in the cells that produce sperm. Germ cell tumors are further divided into two subtypes:
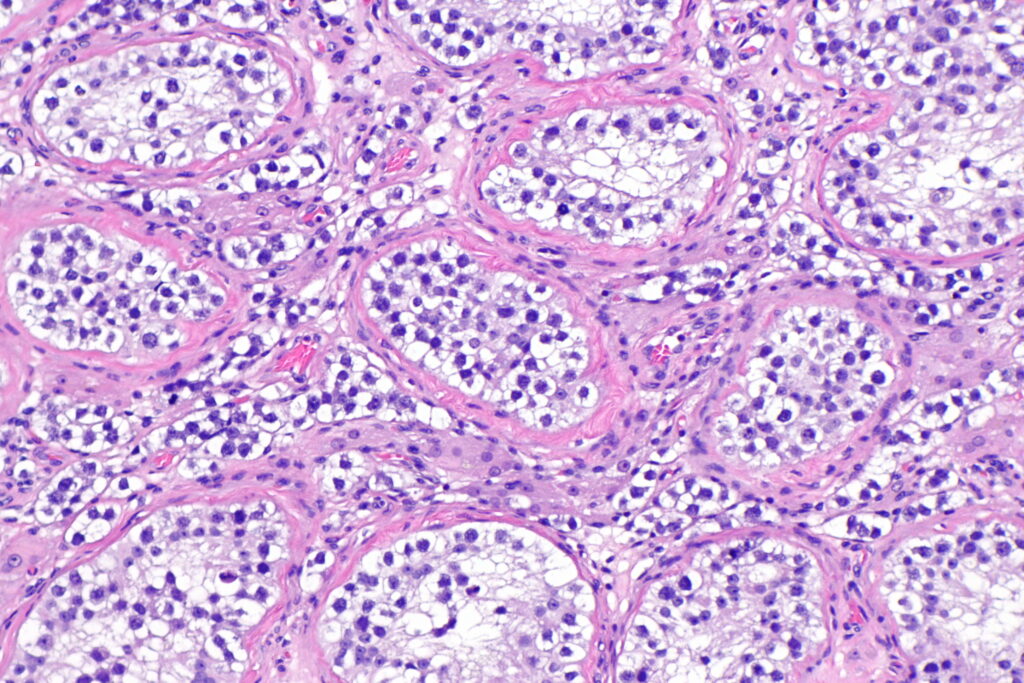
- Seminomas: These tend to grow and spread more slowly compared to other types. They usually respond well to radiation therapy and chemotherapy.
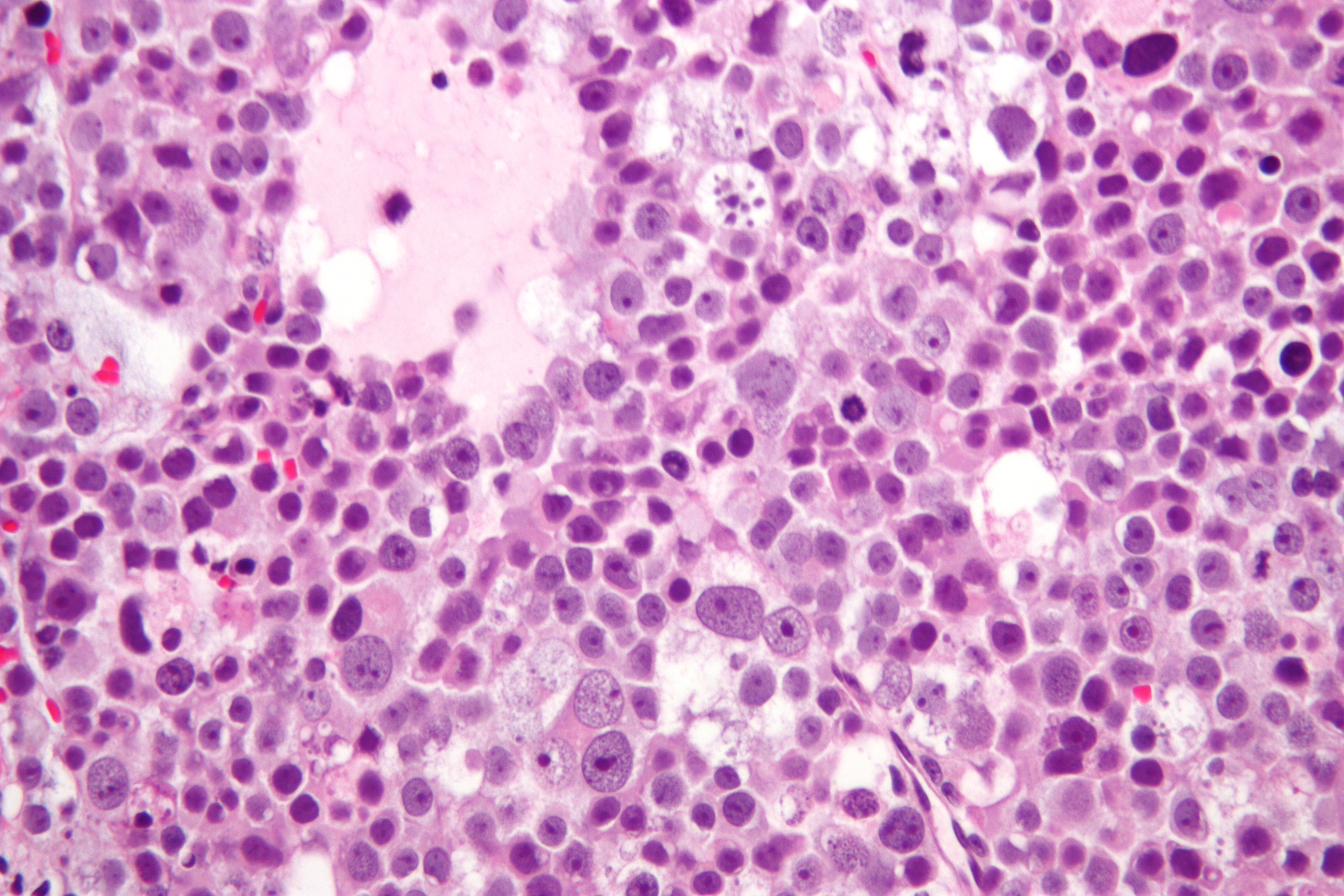
- Nonseminomas: These tumors grow and spread more rapidly. They include several subtypes such as embryonal carcinoma, yolk sac tumor, choriocarcinoma, and teratoma.
- Stromal Tumors: These develop in the supportive tissues of the testicles, such as the Leydig cells or Sertoli cells. Stromal tumors are less common and typically occur in children.
- Secondary Testicular Cancer: This occurs when cancer from another part of the body spreads to the testicles. It is rare but can happen in cases of lymphoma or leukemia.
Causes of Testicular Cancer
The exact cause of testicular cancer remains unknown, but researchers have identified several risk factors that may increase the likelihood of developing this condition. These include:
- Undescended Testicle: Men born with an undescended testicle, a condition known as cryptorchidism, have a higher risk of developing testicular cancer. Even if the testicle is surgically corrected, the risk remains elevated.
- Family History: Having a close relative, such as a father or brother, who has had testicular cancer increases the chances of developing the disease.
- Age: Although it can occur at any age, testicular cancer is most common in young and middle-aged men.
- Race and Ethnicity: White men are more likely to develop testicular cancer than men of other races or ethnicities.
- HIV Infection: Some studies suggest a link between human immunodeficiency virus infection and an increased risk of testicular cancer.
- Previous Testicular Cancer: Men who have had cancer in one testicle are at a higher risk of developing cancer in the other testicle.
Symptoms of Testicular Cancer
Recognizing the symptoms of testicular cancer is crucial for early detection and treatment. Common symptoms include:
- Lump or Swelling: A painless lump or swelling in one of the testicles is often the first noticeable symptom. It is important to note that not all lumps are cancerous, but any unusual change should be evaluated by a healthcare professional.
- Pain or Discomfort: Some men may experience a dull ache or feeling of heaviness in the scrotum or lower abdomen. Pain is not always present, but when it occurs, it should not be ignored.
- Change in Testicle Size or Shape: A noticeable change in the size or shape of a testicle can indicate an underlying issue.
- Fluid Accumulation: An increase in fluid within the scrotum may occur in some cases.
- Breast Enlargement or Tenderness: In rare cases, certain types of testicular cancer can lead to hormonal changes that result in breast enlargement or tenderness.
Diagnosing Testicular Cancer
If testicular cancer is suspected, a healthcare provider will perform a series of tests to confirm the diagnosis. These tests may include:
- Physical Examination: A doctor will examine the testicles for any abnormalities, such as lumps or swelling.
- Ultrasound: An ultrasound of the scrotum uses sound waves to create images of the testicles and surrounding tissues. This helps determine whether a lump is solid or filled with fluid, which can indicate whether it is cancerous.
- Blood Tests: Blood tests are used to measure levels of specific proteins, known as tumor markers, that are produced by certain types of testicular cancer. Elevated levels of these markers can support a diagnosis.
- Biopsy: In rare cases, a small sample of tissue may be removed from the testicle for examination under a microscope. However, biopsies are not commonly performed due to the risk of spreading cancer cells.
Treatment Options for Testicular Cancer
The treatment approach for testicular cancer depends on several factors, including the type and stage of the cancer, as well as the patient’s overall health. Common treatment options include:
Surgery
Surgical removal of the affected testicle, known as orchiectomy, is often the first step in treating testicular cancer. This procedure involves making an incision in the groin to remove the testicle. In some cases, a prosthetic testicle may be inserted to restore the appearance of the scrotum.
Radiation Therapy
Radiation therapy uses high-energy beams to target and destroy cancer cells. It is particularly effective for treating seminomas, as these tumors are highly sensitive to radiation. Radiation therapy may also be used after surgery to eliminate any remaining cancer cells.
Chemotherapy
Chemotherapy involves the use of drugs to kill cancer cells. It is often recommended for nonseminomas or advanced-stage cancers that have spread beyond the testicles. Chemotherapy may be administered before or after surgery, depending on the specific case.
Surveillance
In cases where the cancer is detected early and considered low-risk, a doctor may recommend regular monitoring instead of immediate treatment. This approach, known as surveillance, involves periodic physical exams, blood tests, and imaging studies to ensure the cancer does not return or progress.
Retroperitoneal Lymph Node Dissection
This surgical procedure involves removing lymph nodes in the abdomen to prevent the spread of cancer. It is typically performed in cases where the cancer has spread to nearby lymph nodes.
Living with Testicular Cancer
A diagnosis of testicular cancer can be overwhelming, but many men go on to live healthy, fulfilling lives after treatment. Support from family, friends, and healthcare providers plays a critical role in coping with the emotional and physical challenges of the disease. Additionally, joining a support group or seeking counseling can help individuals navigate their journey.
Preventing Testicular Cancer
While there is no guaranteed way to prevent testicular cancer, certain measures can help reduce the risk or detect the disease early. These include:
- Regular Self-Examinations: Men should perform monthly self-examinations of their testicles to check for any unusual lumps or changes.
- Seeking Medical Attention: Any persistent symptoms or concerns should be promptly discussed with a healthcare provider.
- Managing Risk Factors: Addressing known risk factors, such as an undescended testicle, through medical intervention can help lower the risk of developing cancer.