Temporomandibular Joint Dysfunction, commonly referred to as TMJ Disorder, is a condition that affects the jaw joint and the muscles responsible for jaw movement. This disorder can lead to discomfort, pain, and difficulty in performing everyday activities such as eating or speaking. Understanding its causes, recognizing its symptoms, and exploring available treatments are essential steps toward managing this condition effectively.
What is Temporomandibular Joint Dysfunction?
The temporomandibular joint is one of the most complex joints in the human body. It connects the jawbone to the skull and allows for movements like chewing, talking, and yawning. When this joint becomes dysfunctional, it can result in a range of issues collectively known as Temporomandibular Joint Dysfunction. This condition is not life-threatening, but it can significantly impact an individual’s quality of life if left untreated.
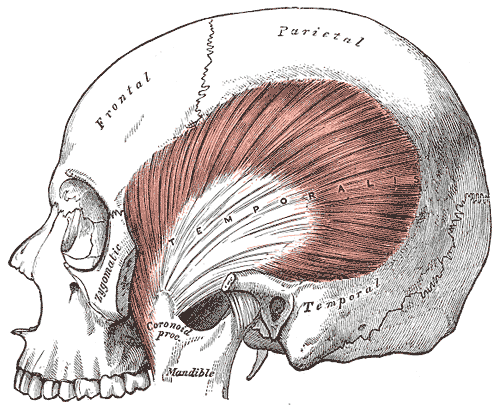
Anatomy of the Jaw Joint
- The Joint Structure: The temporomandibular joint consists of bones, cartilage, and a small disc that acts as a cushion between the bones. This disc ensures smooth movement when opening and closing the mouth.
- Muscles Involved: Several muscles, including the masseter and temporalis, work together to control jaw movement. These muscles are essential for functions like biting and chewing.
Causes of Temporomandibular Joint Dysfunction
There are numerous potential causes of this condition, and often, multiple factors contribute to its development. Below are some of the most common causes:
1. Injury to the Jaw or Joint
Physical trauma to the jaw, such as a blow to the face or whiplash, can damage the joint or surrounding muscles. This injury may lead to misalignment or inflammation, resulting in dysfunction.
2. Arthritis
Arthritis, particularly osteoarthritis or rheumatoid arthritis, can affect the temporomandibular joint. These conditions cause the cartilage within the joint to deteriorate, leading to pain and restricted movement.
3. Teeth Grinding or Clenching
Habitual grinding or clenching of teeth, often during sleep, places excessive pressure on the joint and surrounding muscles. Over time, this can lead to wear and tear, causing dysfunction.
4. Misalignment of the Teeth or Jaw
Poor dental alignment, also known as malocclusion, can place undue stress on the temporomandibular joint. This misalignment forces the joint to work harder than usual, increasing the risk of dysfunction.
5. Stress and Muscle Tension
Stress often manifests physically, causing individuals to tighten their jaw muscles or clench their teeth unconsciously. This tension can strain the joint and exacerbate existing issues.
6. Other Contributing Factors
- Chronic conditions like fibromyalgia or chronic fatigue syndrome
- Poor posture, especially in the neck and upper back
- Connective tissue diseases that affect joint function
Symptoms of Temporomandibular Joint Dysfunction
The symptoms of this condition can vary widely from person to person. Some individuals experience mild discomfort, while others face severe pain and functional limitations. Below are the most common symptoms associated with this disorder:
1. Pain in the Jaw Area
One of the hallmark symptoms is pain or tenderness in the jaw joint. This pain may be localized to the joint itself or radiate to nearby areas such as the ear, temple, or neck.
2. Difficulty Chewing or Biting
Individuals with this condition often find it challenging to chew food comfortably. They may also experience a feeling of the jaw “locking” in an open or closed position.
3. Clicking or Popping Sounds
Audible clicking, popping, or grating sounds when moving the jaw are common signs of dysfunction. While these sounds may not always be painful, they indicate underlying joint issues.
4. Swelling Around the Jaw
Inflammation in the joint area can lead to visible swelling. This swelling may be accompanied by warmth or redness in severe cases.
5. Headaches and Ear Pain
Many people with this condition report frequent headaches, particularly in the temples. Ear pain or a sensation of fullness in the ears is also common, even though there may be no actual ear infection.
6. Limited Jaw Movement
Restricted jaw movement is another significant symptom. Individuals may find it difficult to open their mouths wide or move their jaws side to side without discomfort.
Diagnosing Temporomandibular Joint Dysfunction
Diagnosing this condition requires a thorough evaluation by a healthcare professional. Since its symptoms overlap with other conditions, accurate diagnosis is crucial for effective treatment. Here are the typical steps involved in diagnosing this disorder:
1. Medical History Review
A doctor will begin by reviewing the patient’s medical history, including any previous injuries, dental work, or chronic conditions that may contribute to the issue.
2. Physical Examination
The healthcare provider will examine the jaw joint for signs of swelling, tenderness, or misalignment. They may also listen for clicking or popping sounds during jaw movement.
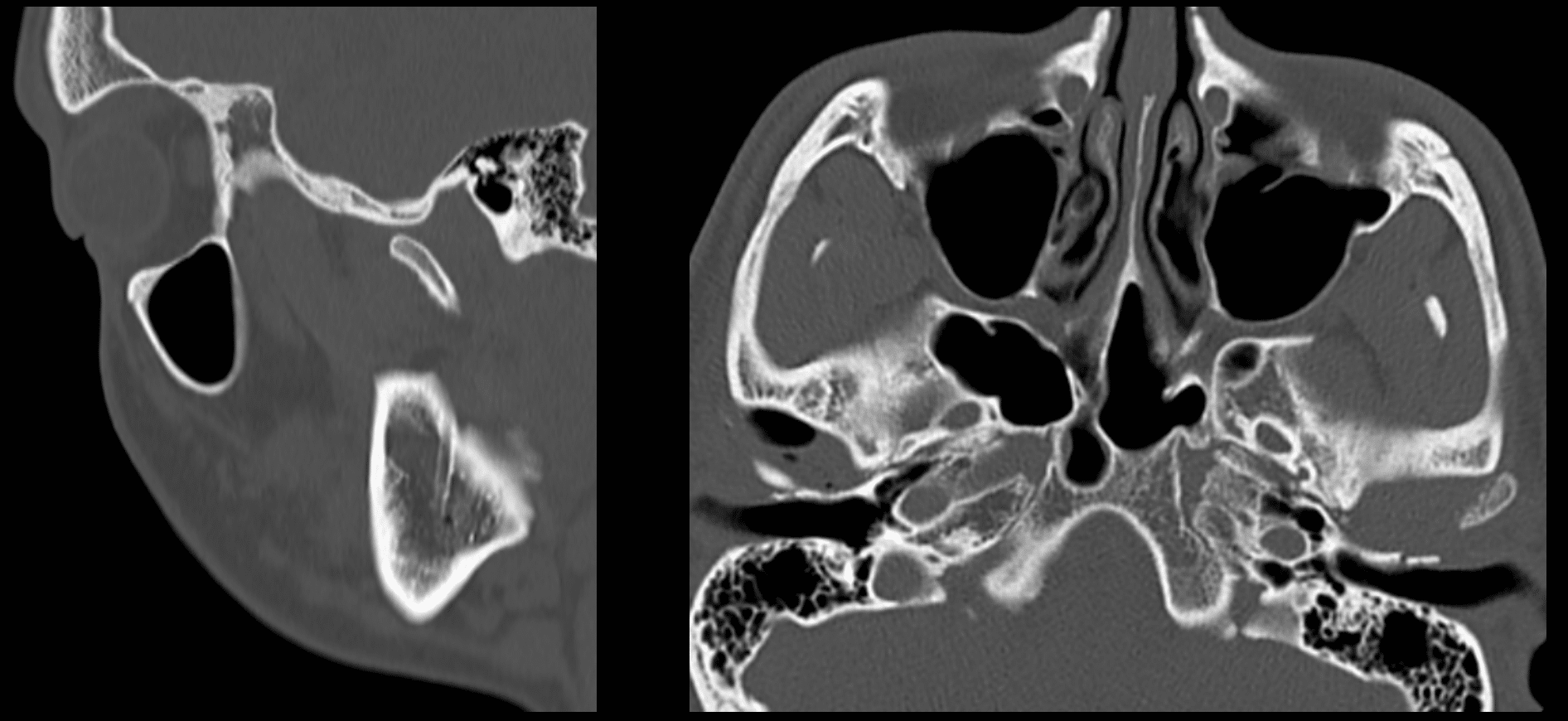
3. Imaging Tests
In some cases, imaging tests such as X-rays, CT scans, or MRI scans may be necessary to assess the joint’s structure and identify any abnormalities.
Treatments for Temporomandibular Joint Dysfunction
Treatment options for this condition depend on the severity of symptoms and the underlying cause. In many cases, conservative measures are sufficient to alleviate discomfort. However, more invasive treatments may be required for persistent or severe cases.
1. Self-Care and Lifestyle Modifications
Simple lifestyle changes can often provide relief for mild cases of this condition:
- Applying Heat or Cold Packs: Alternating heat and cold therapy can reduce pain and inflammation in the joint area.
- Avoiding Hard Foods: Eating soft foods and avoiding hard, chewy, or sticky items can minimize strain on the jaw.
- Practicing Relaxation Techniques: Stress management techniques like meditation or yoga can help reduce muscle tension.
2. Medications
Over-the-counter pain relievers and anti-inflammatory medications are often recommended to manage pain and swelling. In some cases, a doctor may prescribe stronger medications or muscle relaxants for short-term use.
3. Dental Treatments
Dental interventions can address underlying issues contributing to this condition:
- Mouthguards or Splints: Custom-fitted oral appliances can prevent teeth grinding and reduce pressure on the joint.
- Orthodontic Treatment: Correcting misaligned teeth or jaw structures can alleviate stress on the joint.
4. Physical Therapy
Physical therapy exercises can improve jaw mobility and strengthen the surrounding muscles. A physical therapist may also use manual techniques to release tension and improve joint function.
5. Injections
In cases of severe pain, corticosteroid injections may be administered directly into the joint to reduce inflammation. Botox injections are another option for relaxing overactive jaw muscles.
6. Surgical Interventions
Surgery is typically considered a last resort when all other treatments have failed. Surgical options include:
- Arthrocentesis: A minimally invasive procedure to remove fluid and debris from the joint.
- Open Joint Surgery: Reserved for severe cases involving structural damage to the joint.
Preventing Temporomandibular Joint Dysfunction
While not all cases of this condition can be prevented, certain measures can reduce the risk of developing it:
- Maintain good posture, especially when sitting for long periods.
- Avoid habits like nail-biting or chewing on pens, which strain the jaw.
- Seek prompt treatment for dental issues to prevent misalignment.
- Manage stress through relaxation techniques and regular exercise.
When to Seek Professional Help
It is important to consult a healthcare provider if symptoms persist or worsen over time. Persistent pain, difficulty eating, or significant jaw locking are signs that professional intervention may be necessary. Early diagnosis and treatment can prevent complications and improve outcomes.