Temporomandibular Joint Dysfunction, commonly referred to as TMJ Disorder, is a condition that affects the joint connecting the jawbone to the skull. This joint, known as the temporomandibular joint, plays a crucial role in everyday activities such as chewing, speaking, and yawning. When this joint becomes dysfunctional, it can lead to discomfort, pain, and limited movement. In this article, we will explore the causes, symptoms, and treatments associated with this condition.
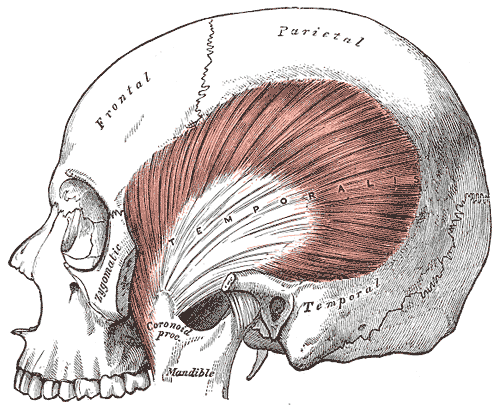
Understanding the Temporomandibular Joint
The temporomandibular joint is one of the most complex joints in the human body. It acts as a sliding hinge, allowing the jaw to move up and down, side to side, and forward and backward. The joint consists of bones, muscles, ligaments, and a small disc that cushions the joint and ensures smooth movement. When any part of this intricate system is disrupted, it can result in dysfunction and discomfort.
Anatomy of the Joint
- Bones: The joint connects the temporal bone of the skull with the mandible, or lower jawbone.
- Muscles: Various muscles, including the masseter and temporalis, help control jaw movement.
- Ligaments: These fibrous tissues stabilize the joint and prevent excessive movement.
- Disc: A small, flexible disc acts as a cushion between the bones, ensuring smooth motion.
Common Causes of Dysfunction
There are several factors that can contribute to dysfunction in the temporomandibular joint. Understanding these causes is essential for effective diagnosis and treatment.
Trauma or Injury
Injuries to the jaw, head, or neck can damage the joint or surrounding muscles, leading to dysfunction. For example, a direct blow to the jaw during an accident or sports activity can displace the disc or cause inflammation in the joint.
Arthritis
Conditions such as osteoarthritis or rheumatoid arthritis can affect the temporomandibular joint. Arthritis causes the cartilage in the joint to deteriorate, resulting in pain and stiffness.
Bruxism
Bruxism, or teeth grinding, is a common cause of dysfunction. This habit often occurs during sleep and puts excessive pressure on the joint and surrounding muscles, leading to soreness and discomfort.
Poor Posture
Poor posture, particularly in the neck and upper back, can strain the muscles connected to the temporomandibular joint. Over time, this strain can contribute to dysfunction and pain.
Stress and Anxiety
Stress and anxiety can lead to clenching of the jaw or teeth grinding, both of which place additional stress on the joint. Chronic stress may also cause muscle tension in the face and neck, exacerbating symptoms.
Malocclusion
Malocclusion, or misalignment of the teeth, can disrupt the natural movement of the jaw. This misalignment forces the joint to work harder, increasing the risk of dysfunction.
Symptoms of Dysfunction
The symptoms of dysfunction in the temporomandibular joint can vary widely from person to person. Some individuals experience mild discomfort, while others may have severe pain and limited jaw movement. Below are some of the most common symptoms.
Jaw Pain
Pain in the jaw is one of the hallmark symptoms of dysfunction. This pain may be localized to the joint itself or radiate to nearby areas, such as the ear, temple, or neck.
Clicking or Popping Sounds
Many individuals with dysfunction report hearing clicking, popping, or grating sounds when they move their jaw. These noises are often caused by the displacement of the disc within the joint.
Difficulty Chewing
Chewing can become difficult or painful due to stiffness or misalignment of the joint. Some people may also notice a feeling of fatigue in the jaw muscles after eating.
Locking of the Jaw
In severe cases, the jaw may lock in an open or closed position. This can make it challenging to speak, eat, or perform other daily activities.
Headaches
Frequent headaches, particularly in the temples, are a common symptom. These headaches are often tension-related and may worsen with prolonged jaw clenching or grinding.
Ear Pain or Tinnitus
Some individuals experience ear pain, ringing in the ears (tinnitus), or a feeling of fullness in the ear. These symptoms occur because the temporomandibular joint is located close to the ear canal.
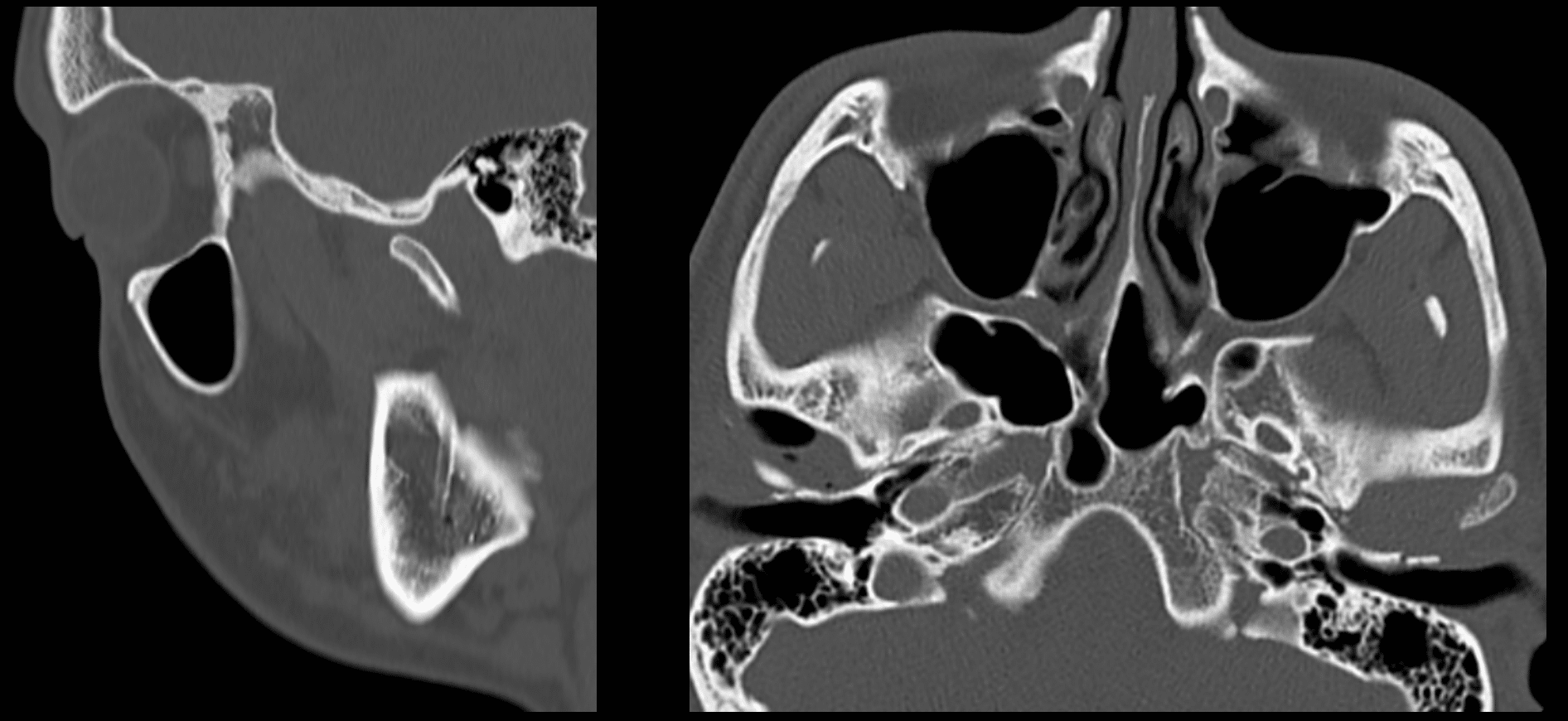
Diagnosis of Dysfunction
Diagnosing dysfunction in the temporomandibular joint typically involves a combination of physical examination, medical history review, and imaging tests. A healthcare professional will assess the range of motion in the jaw, listen for unusual sounds, and check for areas of tenderness. Imaging tests, such as X-rays, MRI scans, or CT scans, may be used to examine the joint and surrounding structures in greater detail.
Treatment Options
Treatment for dysfunction in the temporomandibular joint focuses on relieving pain, improving jaw function, and addressing underlying causes. The approach to treatment depends on the severity of symptoms and the specific factors contributing to the dysfunction.
Lifestyle Modifications
Making certain lifestyle changes can help alleviate symptoms and prevent further issues. These modifications include:
- Avoiding hard or chewy foods that strain the jaw.
- Practicing good posture to reduce strain on the neck and jaw muscles.
- Using relaxation techniques, such as deep breathing or meditation, to manage stress.
Dental Appliances
Dental appliances, such as mouthguards or splints, are often recommended to prevent teeth grinding and reduce pressure on the joint. These devices are custom-fitted by a dentist and worn during sleep or throughout the day as needed.
Physical Therapy
Physical therapy can be highly effective in treating dysfunction. A physical therapist may use manual techniques to improve joint mobility and teach exercises to strengthen the jaw muscles. Heat or cold therapy may also be applied to reduce pain and inflammation.
Medications
Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help manage mild to moderate pain. In more severe cases, a doctor may prescribe muscle relaxants or anti-inflammatory medications to address persistent symptoms.
Injections
Corticosteroid injections may be administered directly into the joint to reduce inflammation and relieve pain. In some cases, botulinum toxin (Botox) injections are used to relax overactive jaw muscles.
Surgical Interventions
Surgery is typically considered a last resort when conservative treatments fail to provide relief. Surgical options include arthrocentesis, which involves flushing out the joint to remove debris, or more invasive procedures such as joint replacement surgery.
Preventing Dysfunction
While not all cases of dysfunction can be prevented, certain measures can reduce the risk of developing this condition. Maintaining good oral health, avoiding excessive gum chewing, and seeking prompt treatment for injuries or dental issues can help protect the joint. Additionally, managing stress and practicing relaxation techniques can minimize the impact of clenching or grinding habits.
When to Seek Medical Attention
If you experience persistent jaw pain, difficulty opening or closing your mouth, or other concerning symptoms, it is important to consult a healthcare professional. Early diagnosis and treatment can prevent complications and improve quality of life.