Tay-Sachs Disease, often abbreviated as TSD, is a rare and devastating genetic condition that primarily affects infants and young children. This disorder is caused by the absence or malfunction of an essential enzyme, leading to severe neurological damage and, ultimately, premature death. Despite its rarity, Tay-Sachs Disease has become a focal point for understanding genetic disorders, inheritance patterns, and the importance of genetic counseling. In this article, we will delve into the causes, symptoms, diagnosis, and potential treatments for this tragic condition.

What is Tay-Sachs Disease?
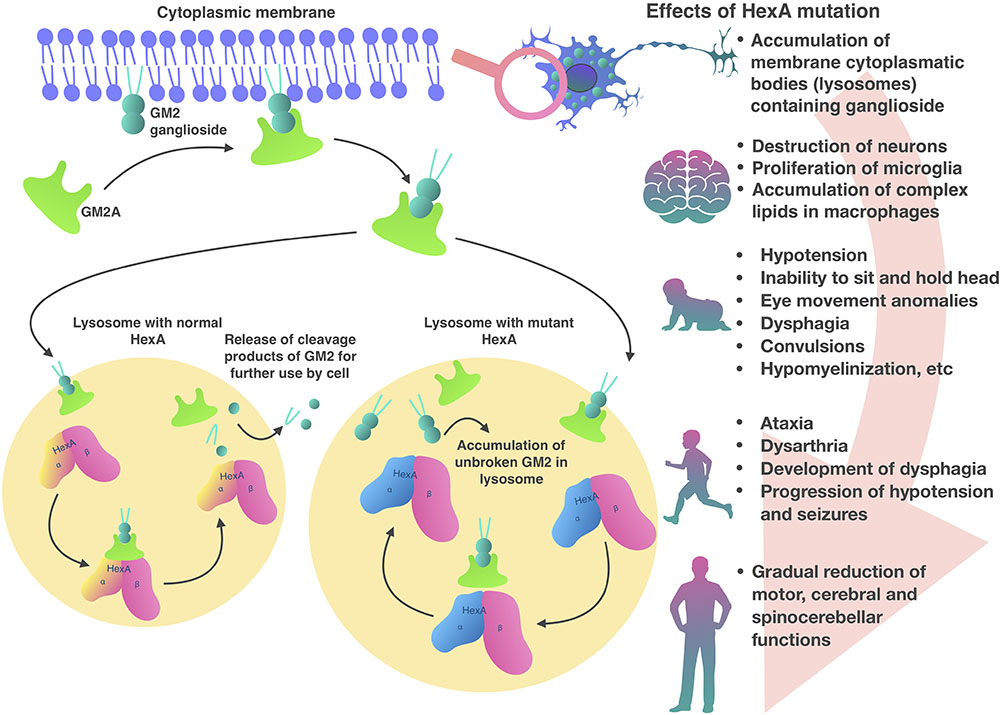
Tay-Sachs Disease is a hereditary disorder that belongs to a group of conditions known as lysosomal storage diseases. It occurs when there is a deficiency in an enzyme called hexosaminidase A. This enzyme plays a critical role in breaking down a fatty substance called GM2 ganglioside, which accumulates in the nerve cells of the brain and spinal cord. Over time, this buildup leads to progressive damage to the nervous system.
The disease was first described in the late 19th century by British ophthalmologist Warren Tay and American neurologist Bernard Sachs. While Tay observed the characteristic cherry-red spot in the retina of affected individuals, Sachs identified the cellular changes associated with the disorder. Their combined work laid the foundation for our current understanding of this condition.
Types of Tay-Sachs Disease
Tay-Sachs Disease can manifest in different forms, depending on the age of onset and severity of symptoms:
- Infantile Tay-Sachs Disease: The most common and severe form, typically appearing in infants around three to six months of age.
- Juvenile Tay-Sachs Disease: A less severe form that begins in childhood, usually between the ages of two and ten years.
- Late-Onset Tay-Sachs Disease: A milder form that develops in adolescence or adulthood, with symptoms progressing more slowly.
Causes of Tay-Sachs Disease
Tay-Sachs Disease is caused by mutations in the HEXA gene, which provides instructions for producing the hexosaminidase A enzyme. When both copies of this gene are mutated—one inherited from each parent—the body cannot produce enough functional enzyme to break down GM2 ganglioside. As a result, this fatty substance accumulates in the lysosomes of nerve cells, causing them to swell and eventually die.
Inheritance Pattern
This condition follows an autosomal recessive inheritance pattern. This means that both parents must carry a mutated copy of the HEXA gene for their child to be at risk of developing the disease. Carriers of a single mutated gene typically do not show any symptoms but have a 25 percent chance of passing the disorder to their offspring if both parents are carriers.
Symptoms of Tay-Sachs Disease
The symptoms of Tay-Sachs Disease vary depending on the type and age of onset. However, all forms share a common feature: progressive neurological deterioration.
Infantile Tay-Sachs Disease Symptoms
Infants with this form of the disease appear healthy at birth but begin to exhibit symptoms within the first few months of life. These symptoms include:
- Loss of motor skills, such as rolling over, sitting, and crawling
- Decreased muscle tone (hypotonia)
- Increased startle reflex
- Vision problems, including the characteristic cherry-red spot in the retina
- Seizures
- Developmental delays
Juvenile Tay-Sachs Disease Symptoms
Children with juvenile Tay-Sachs Disease may experience a slower progression of symptoms compared to the infantile form. Common signs include:
- Difficulty walking and coordination problems
- Speech difficulties
- Muscle weakness
- Behavioral changes
- Intellectual disability
Late-Onset Tay-Sachs Disease Symptoms
In the adult form, symptoms develop gradually and may include:
- Muscle weakness and cramping
- Tremors
- Slurred speech
- Mood changes and psychiatric symptoms
- Cognitive decline
Diagnosis of Tay-Sachs Disease
Early diagnosis of Tay-Sachs Disease is crucial for providing appropriate care and support to affected individuals and their families. Several methods are used to diagnose this condition:
Prenatal Testing
Prenatal testing can identify Tay-Sachs Disease before birth. This is particularly important for couples who are known carriers of the mutated gene. Two common prenatal tests include:
- Amniocentesis: A procedure in which a small sample of amniotic fluid is taken and analyzed for enzyme activity and genetic mutations.
- Chorionic Villus Sampling: A test that involves taking a sample of placental tissue to detect genetic abnormalities.
Newborn Screening
While Tay-Sachs Disease is not routinely included in standard newborn screening panels in many countries, specialized tests can be performed if there is a family history or suspicion of the disorder.
Enzyme Assays
Enzyme assays measure the activity of hexosaminidase A in blood or tissue samples. Low or absent enzyme activity strongly suggests the presence of Tay-Sachs Disease.
Genetic Testing
Genetic testing can confirm a diagnosis by identifying mutations in the HEXA gene. This method is also useful for carrier screening, especially in populations with a higher prevalence of the disease.
Treatment Options for Tay-Sachs Disease
Unfortunately, there is currently no cure for Tay-Sachs Disease. Treatment focuses on managing symptoms and improving the quality of life for affected individuals and their families.
Supportive Care
Supportive care is the cornerstone of treatment for Tay-Sachs Disease. This includes:
- Physical Therapy: To maintain mobility and prevent joint stiffness.
- Occupational Therapy: To help individuals perform daily activities as independently as possible.
- Speech Therapy: To address communication challenges.
- Nutritional Support: To ensure adequate nutrition, especially in cases where swallowing becomes difficult.
Medications
Medications may be prescribed to manage specific symptoms, such as seizures or muscle spasms. However, these treatments do not address the underlying cause of the disease.
Experimental Therapies
Researchers are actively exploring potential treatments for Tay-Sachs Disease, including:
- Gene Therapy: An experimental approach that aims to introduce a functional copy of the HEXA gene into affected cells.
- Substrate Reduction Therapy: A strategy that reduces the production of GM2 ganglioside to slow its accumulation.
- Enzyme Replacement Therapy: Attempts to replace the missing enzyme, although delivering it to the brain remains a significant challenge.
Living with Tay-Sachs Disease
For families affected by Tay-Sachs Disease, the emotional and financial burden can be overwhelming. Support groups, counseling services, and educational resources are available to help navigate the challenges of living with this condition.
Importance of Genetic Counseling
Genetic counseling plays a vital role in helping individuals and families understand the risks and implications of Tay-Sachs Disease. Counselors provide information about inheritance patterns, carrier testing, and reproductive options, empowering families to make informed decisions.
Raising Awareness
Raising awareness about Tay-Sachs Disease is essential for promoting early diagnosis, advancing research, and supporting affected families. Public education campaigns and advocacy efforts aim to reduce stigma and encourage funding for scientific studies.