Sweets Syndrome, also known as Acute Febrile Neutrophilic Dermatosis, is a rare inflammatory condition that primarily affects the skin. First described by Dr. Robert Douglas Sweet in 1964, this syndrome has intrigued medical professionals due to its unique presentation and association with systemic diseases. While it is most commonly recognized for its distinct skin manifestations, Sweets Syndrome can also involve other organs and systems in the body. This article delves into the symptoms, causes, and treatment options available for individuals affected by this condition.
Understanding Sweets Syndrome
Sweets Syndrome is characterized by the sudden onset of fever, elevated white blood cell count, and painful skin lesions. These lesions typically appear as red or purple bumps or plaques, often on the arms, face, neck, or legs. The condition is classified into three main types: classical, malignancy-associated, and drug-induced. Each type has its own set of triggers and underlying factors, which will be explored further in subsequent sections.
Symptoms of Sweets Syndrome
The symptoms of Sweets Syndrome can vary from person to person but generally include a combination of systemic and dermatological signs. Below is a detailed breakdown of the most common symptoms:
Fever and General Malaise
- Many individuals with Sweets Syndrome experience a sudden onset of fever, often accompanied by fatigue and general discomfort.
- This fever is typically high-grade and may persist until appropriate treatment is initiated.
Painful Skin Lesions
- The hallmark of Sweets Syndrome is the development of tender, raised, red or purple skin lesions.
- These lesions can vary in size and may appear singly or in clusters.
- They are often found on the arms, face, neck, and legs but can occur anywhere on the body.
Inflammation and Swelling
- In addition to skin lesions, some patients may experience swelling in the affected areas.
- This inflammation can contribute to the pain and discomfort associated with the condition.
Other Systemic Symptoms
- Some individuals may develop joint pain, muscle aches, or headaches.
- In rare cases, internal organs such as the eyes, kidneys, or lungs may be involved, leading to more severe complications.
Causes and Triggers of Sweets Syndrome
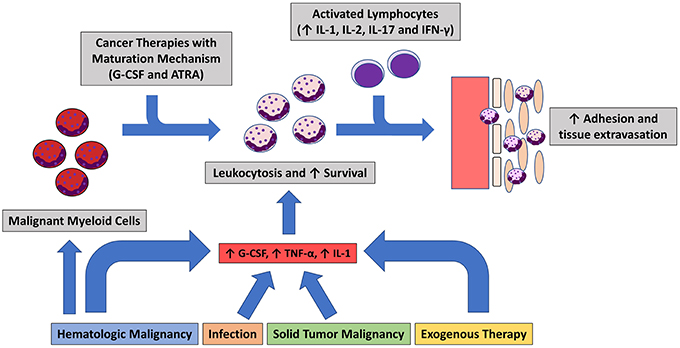
While the exact cause of Sweets Syndrome remains unknown, researchers have identified several potential triggers and associations. These triggers can be broadly categorized into three groups: classical, malignancy-associated, and drug-induced.
Classical Sweets Syndrome
- Classical Sweets Syndrome often occurs in otherwise healthy individuals and is frequently preceded by an upper respiratory infection or gastrointestinal illness.
- It is believed to result from an abnormal immune response, where the body’s immune system mistakenly attacks its own tissues.
Malignancy-Associated Sweets Syndrome
- In some cases, Sweets Syndrome is linked to underlying cancers, particularly blood-related malignancies such as leukemia or lymphoma.
- The appearance of skin lesions may precede the diagnosis of cancer, making it an important diagnostic clue for healthcare providers.
Drug-Induced Sweets Syndrome
- Certain medications, including antibiotics, nonsteroidal anti-inflammatory drugs, and granulocyte colony-stimulating factors, have been implicated in triggering Sweets Syndrome.
- The onset of symptoms typically occurs within days to weeks after starting the medication.
Diagnosis of Sweets Syndrome
Diagnosing Sweets Syndrome requires a thorough evaluation by a healthcare professional. Several criteria must be met to confirm the diagnosis, including clinical findings, laboratory tests, and sometimes a biopsy of the skin lesions.
Clinical Criteria
- The presence of characteristic skin lesions, fever, and elevated white blood cell count are key indicators.
- A detailed medical history and physical examination are essential to rule out other conditions with similar presentations.
Laboratory Tests
- Blood tests may reveal an increase in neutrophils, a type of white blood cell associated with inflammation.
- Additional tests may be conducted to check for underlying infections, autoimmune disorders, or malignancies.
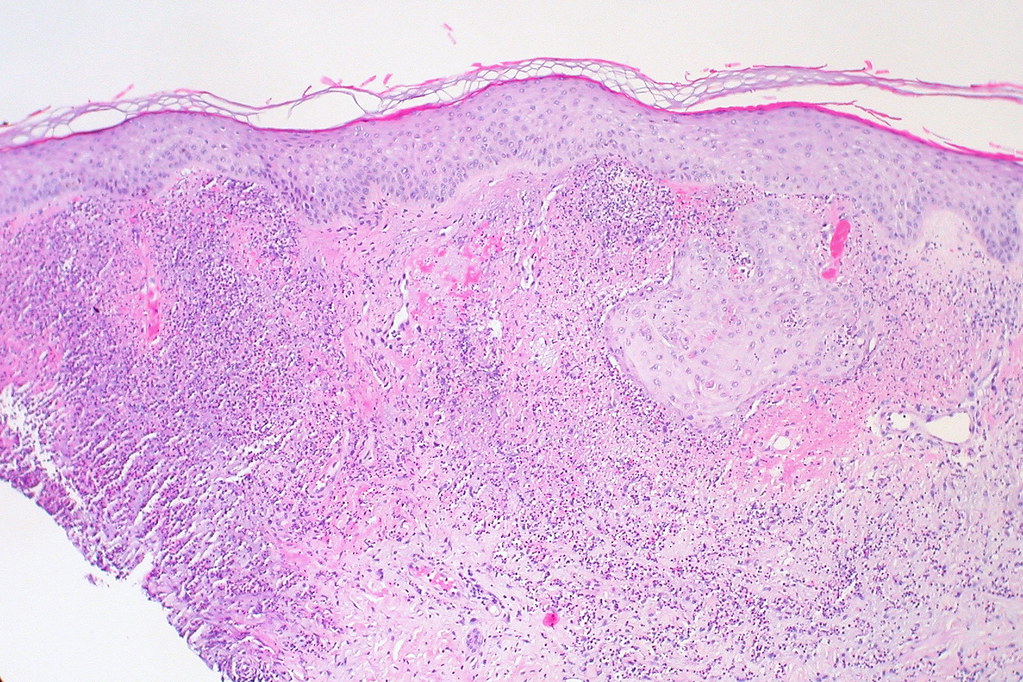
Skin Biopsy
- A biopsy of the skin lesion can provide definitive evidence of Sweets Syndrome.
- Under the microscope, the biopsy typically shows an infiltration of neutrophils in the upper layers of the skin.
Treatment Options for Sweets Syndrome
Fortunately, Sweets Syndrome is highly responsive to treatment, and many individuals experience rapid improvement once therapy is initiated. The choice of treatment depends on the severity of symptoms, the underlying cause, and the patient’s overall health.
Corticosteroids
- Corticosteroids, such as prednisone, are the mainstay of treatment for Sweets Syndrome.
- These medications work by suppressing the immune system and reducing inflammation.
- Oral corticosteroids are typically prescribed, but in severe cases, intravenous administration may be necessary.
Topical Treatments
- For mild cases or localized lesions, topical corticosteroid creams or ointments may be sufficient.
- These treatments help reduce inflammation and alleviate discomfort without the systemic side effects of oral medications.
Alternative Therapies
- In cases where corticosteroids are contraindicated or ineffective, alternative therapies such as colchicine, dapsone, or potassium iodide may be considered.
- These medications target different pathways of inflammation and can be effective in certain patients.
Treating Underlying Conditions
- If Sweets Syndrome is associated with an underlying condition, such as cancer or an infection, treating the primary disease is crucial.
- Addressing the root cause can lead to resolution of the syndrome and prevent recurrence.
Prognosis and Long-Term Management
The prognosis for individuals with Sweets Syndrome is generally favorable, especially when the condition is promptly diagnosed and treated. Most patients experience complete resolution of symptoms within weeks to months. However, recurrence is possible, particularly in cases associated with malignancies or chronic conditions.
Monitoring and Follow-Up
- Regular follow-up appointments with a healthcare provider are important to monitor for recurrence or complications.
- Patients should report any new or worsening symptoms promptly to ensure timely intervention.
Lifestyle Modifications
- Maintaining a healthy lifestyle, including a balanced diet and regular exercise, can support overall immune function.
- Avoiding known triggers, such as certain medications, may help reduce the risk of recurrence.
Raising Awareness and Support
Due to its rarity, Sweets Syndrome is not widely understood by the general public or even some healthcare providers. Raising awareness about the condition can help improve early diagnosis and access to appropriate care. Support groups and online communities can provide valuable resources and emotional support for individuals and families affected by this condition.