A subdural hematoma, often abbreviated as SDH, is a serious medical condition that occurs when blood collects between the layers of tissue surrounding the brain. This condition can develop rapidly or over time, depending on the underlying cause and severity. Understanding the causes, recognizing the symptoms, obtaining an accurate diagnosis, and pursuing appropriate treatment are essential steps in managing this potentially life-threatening condition.

What Is a Subdural Hematoma?
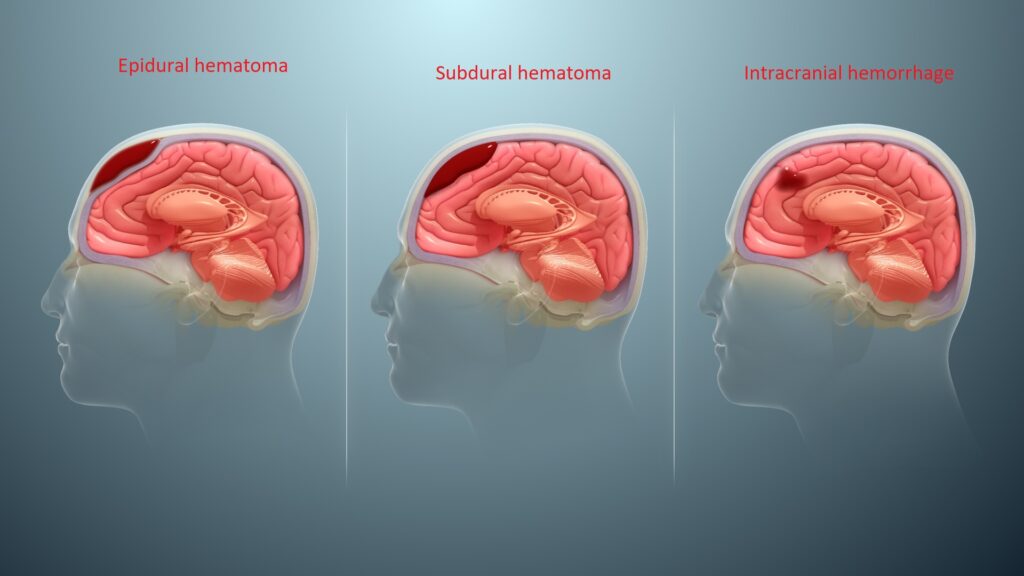
A subdural hematoma happens when blood accumulates in the space between the dura mater, which is the outermost protective layer of the brain, and the arachnoid mater, the middle layer. This accumulation puts pressure on the brain, which can lead to significant neurological problems if not treated promptly. Subdural hematomas are typically classified into two main types based on their onset and progression: acute and chronic.
Acute Subdural Hematoma
An acute subdural hematoma develops quickly, often within hours or days after a head injury. This type is usually associated with severe trauma, such as a car accident or a fall from a significant height. Acute subdural hematomas are considered medical emergencies because they can cause rapid deterioration of brain function.
Chronic Subdural Hematoma
In contrast, a chronic subdural hematoma develops more slowly, sometimes taking weeks or even months to manifest symptoms. This type is more common in older adults, particularly those who take blood-thinning medications or have conditions that make them prone to bleeding. Chronic subdural hematomas may result from minor head injuries that go unnoticed at the time.
Causes of Subdural Hematoma
The primary cause of a subdural hematoma is trauma to the head. However, other factors can contribute to its development, especially in cases where no significant injury is apparent.
Head Injuries
- Falls: Falls are one of the most common causes of head injuries leading to subdural hematomas. This is especially true for older adults, who may be more susceptible to falls due to balance issues or frailty.
- Car Accidents: High-impact collisions can cause significant trauma to the head, resulting in bleeding between the layers of brain tissue.
- Sports Injuries: Contact sports like football or boxing carry a risk of head injuries that could lead to a subdural hematoma.
Blood-Thinning Medications
Individuals who take medications to prevent blood clots, such as warfarin or aspirin, are at an increased risk of developing a subdural hematoma. These medications reduce the blood’s ability to clot, making it easier for bleeding to occur even after minor trauma.
Age-Related Factors
As people age, the brain naturally shrinks, creating more space between the brain and the dura mater. This increased space makes the veins connecting these layers more vulnerable to tearing, even with minimal impact. Older adults are therefore more likely to develop chronic subdural hematomas.
Underlying Medical Conditions
Certain medical conditions can predispose individuals to subdural hematomas. For example, people with alcohol use disorder may experience frequent falls and have impaired clotting mechanisms. Similarly, those with conditions like hemophilia or liver disease may have difficulty forming blood clots, increasing their risk of bleeding.
Symptoms of Subdural Hematoma
The symptoms of a subdural hematoma vary depending on whether it is acute or chronic. Recognizing these symptoms early can significantly improve outcomes.
Symptoms of Acute Subdural Hematoma
- Severe Headache: A sudden, intense headache is often one of the first signs of an acute subdural hematoma.
- Confusion or Loss of Consciousness: Individuals may appear disoriented or lose consciousness shortly after the injury.
- Nausea and Vomiting: These symptoms are common and may indicate increased pressure within the skull.
- Seizures: Seizures can occur as a result of the pressure on the brain.
- Weakness or Numbness: Some individuals may experience weakness or numbness on one side of the body.
Symptoms of Chronic Subdural Hematoma
- Mild Headache: Unlike the severe headache associated with acute cases, chronic subdural hematomas often present with a mild, persistent headache.
- Memory Problems: Individuals may notice difficulty remembering recent events or performing routine tasks.
- Changes in Behavior: Personality changes, irritability, or confusion may occur over time.
- Balancing Issues: Difficulty walking or maintaining balance is a common symptom.
Diagnosis of Subdural Hematoma
Diagnosing a subdural hematoma requires a combination of clinical evaluation and imaging studies. Prompt and accurate diagnosis is crucial for effective treatment.
Medical History and Physical Examination
Doctors will begin by asking about any recent head injuries, even minor ones, and assessing the individual’s symptoms. During the physical examination, they will check for signs of neurological impairment, such as weakness, confusion, or abnormal reflexes.
Imaging Studies
- Computed Tomography (CT) Scan: A CT scan is the most commonly used imaging test to diagnose a subdural hematoma. It provides detailed images of the brain and can quickly identify areas of bleeding.
- Magnetic Resonance Imaging (MRI): An MRI may be used in cases where the CT scan results are inconclusive or when a chronic subdural hematoma is suspected. MRI provides more detailed images of soft tissues and can detect smaller bleeds.
Laboratory Tests
In some cases, doctors may order blood tests to assess clotting function, especially if the individual is taking blood-thinning medications. These tests help determine the risk of further bleeding and guide treatment decisions.
Treatment of Subdural Hematoma
The treatment approach for a subdural hematoma depends on its severity, size, and the individual’s overall health. Both surgical and non-surgical options are available, and the choice of treatment is tailored to each case.
Non-Surgical Treatment
For small, asymptomatic chronic subdural hematomas, doctors may opt for observation rather than immediate intervention. This approach involves regular monitoring through imaging studies to ensure the hematoma does not grow or cause symptoms.
Medications
- Pain Relievers: Over-the-counter pain medications may be prescribed to manage headaches or discomfort.
- Anti-Seizure Medications: If seizures occur, medications to control them may be necessary.
Surgical Treatment
Surgery is often required for larger or symptomatic subdural hematomas to relieve pressure on the brain and prevent further complications.
Burr Hole Drainage
This minimally invasive procedure involves drilling small holes into the skull to drain the accumulated blood. Burr hole drainage is commonly used for chronic subdural hematomas and has a high success rate.
Craniotomy
In cases of acute subdural hematomas or when the bleeding is extensive, a craniotomy may be performed. This procedure involves removing a portion of the skull to access and remove the blood clot. A craniotomy is more invasive but may be necessary to prevent permanent brain damage.
Post-Surgical Care
After surgery, individuals are closely monitored in the hospital to ensure proper recovery. Follow-up imaging studies are conducted to confirm that the hematoma has resolved and to check for any complications.
Prevention of Subdural Hematoma
While not all subdural hematomas can be prevented, certain measures can reduce the risk of head injuries and subsequent bleeding.
Safety Precautions
- Wear Helmets: Helmets should be worn during activities like cycling, skateboarding, or contact sports to protect the head from injury.
- Fall Prevention: Installing handrails, using non-slip mats, and ensuring adequate lighting can help prevent falls, especially for older adults.
Medication Management
Individuals taking blood-thinning medications should work closely with their healthcare providers to monitor their dosage and minimize the risk of bleeding. Regular blood tests may be necessary to ensure clotting levels remain within a safe range.
Regular Check-Ups
Older adults and those with underlying medical conditions should undergo regular medical check-ups to address any potential risk factors for subdural hematomas. Early detection and management of these factors can help prevent complications.