Squamous cell carcinoma, often abbreviated as SCC, is one of the most common forms of skin cancer. It originates in the squamous cells, which are flat, thin cells found in the outermost layer of the skin. While it is generally less aggressive than melanoma, it can still spread to other parts of the body if left untreated. This article explores the causes, symptoms, diagnosis, and treatment options for this condition.
Understanding Squamous Cell Skin Cancer
Squamous cell skin cancer develops when the DNA of squamous cells becomes damaged, leading to uncontrolled growth. These cells are located in the epidermis, the topmost layer of the skin. The cancer typically appears on areas of the body that are frequently exposed to sunlight, such as the face, ears, neck, arms, and hands. However, it can also occur in other areas, including mucous membranes and genital regions.
Causes of Squamous Cell Skin Cancer
Several factors contribute to the development of squamous cell skin cancer. Understanding these causes can help individuals take preventive measures to reduce their risk.
Exposure to Ultraviolet Radiation
- Sunlight: Prolonged exposure to ultraviolet rays from the sun is one of the primary causes of squamous cell skin cancer. UV radiation damages the DNA in skin cells, leading to mutations that can result in cancer.
- Tanning Beds: Artificial sources of ultraviolet radiation, such as tanning beds, also increase the risk of developing this type of skin cancer. Using tanning beds before the age of thirty significantly raises the likelihood of developing squamous cell carcinoma later in life.
Weakened Immune System
A compromised immune system can make individuals more susceptible to squamous cell skin cancer. People with conditions like human immunodeficiency virus or those undergoing organ transplants and taking immunosuppressive medications are at higher risk. The immune system plays a critical role in identifying and destroying abnormal cells, so any impairment can allow cancerous cells to grow unchecked.
Fair Skin and Genetic Factors
- Fair Skin: Individuals with fair skin have less melanin, the pigment that provides some protection against ultraviolet radiation. As a result, they are more vulnerable to the harmful effects of UV rays.
- Family History: A family history of skin cancer increases the risk of developing squamous cell carcinoma. Certain genetic disorders, such as xeroderma pigmentosum, which impairs the ability to repair DNA damage caused by UV radiation, also elevate the risk.
Chronic Skin Inflammation and Scarring
Long-term skin inflammation or scarring from burns, infections, or other skin conditions can predispose individuals to squamous cell skin cancer. For example, people with chronic ulcers or scars from severe burns may develop this type of cancer in the affected areas.
Symptoms of Squamous Cell Skin Cancer
Recognizing the symptoms of squamous cell skin cancer early can lead to prompt diagnosis and treatment. The following signs should not be ignored:
Changes in Skin Appearance
- Rough or Scaly Patches: These patches may appear red, pink, or brown and feel rough to the touch. They often develop on sun-exposed areas of the skin.
- Firm Red Nodules: Raised, dome-shaped nodules that may crust or bleed are another common symptom. These lesions are often painless but can become tender over time.
Non-Healing Sores
Squamous cell skin cancer can present as open sores that do not heal or repeatedly bleed and scab. These sores may appear on the lips, inside the mouth, or on the genitals, making them easy to overlook.
Growth with Irregular Borders
Some cases of squamous cell skin cancer manifest as irregularly shaped growths with uneven borders. These growths may expand slowly over time and sometimes develop into ulcers.
Diagnosis of Squamous Cell Skin Cancer
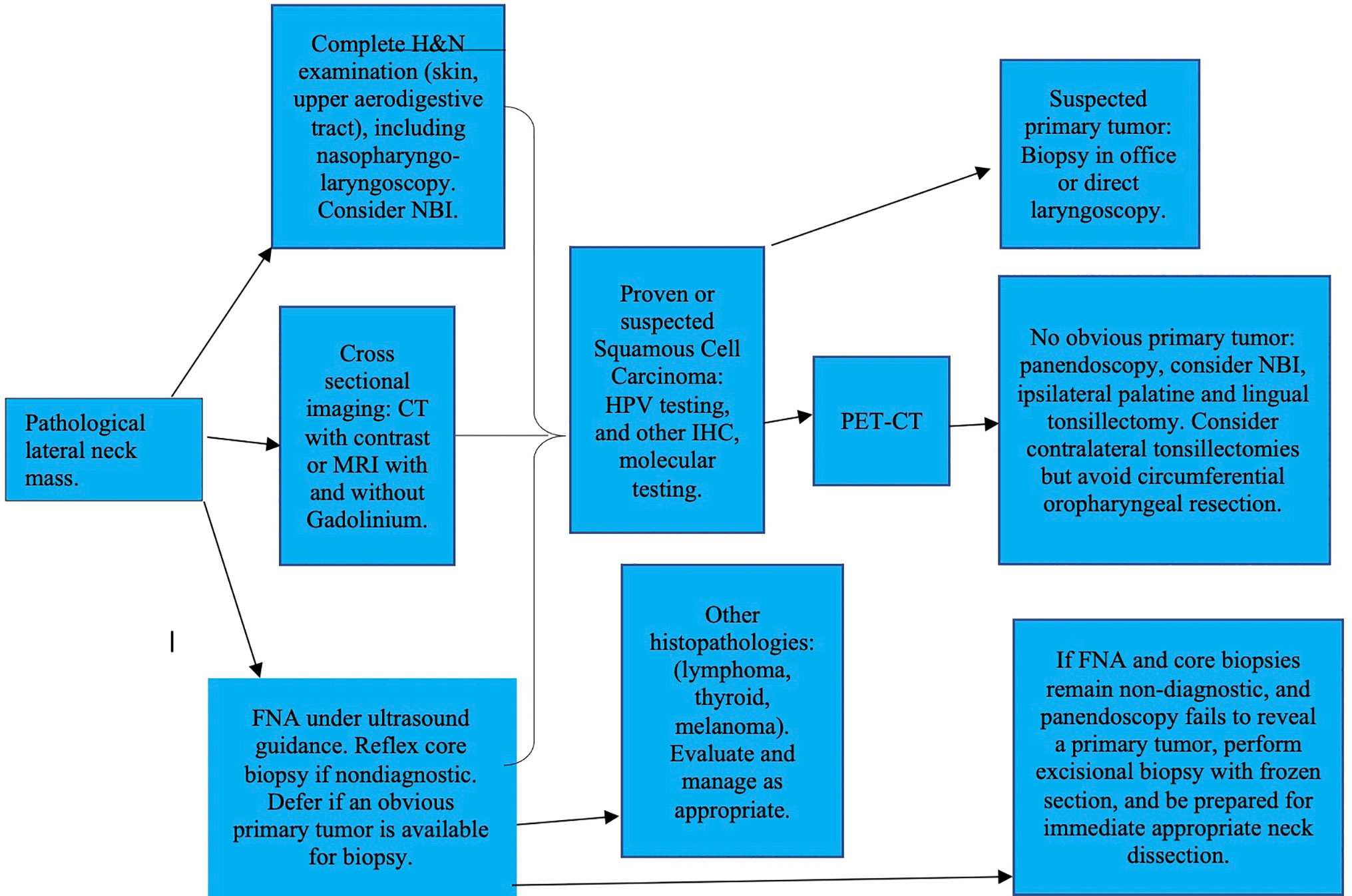
If squamous cell skin cancer is suspected, a healthcare provider will perform a series of diagnostic tests to confirm the presence of the disease and determine its severity.
Physical Examination
The first step in diagnosing squamous cell skin cancer involves a thorough physical examination. During this process, the doctor will inspect the skin for suspicious lesions, paying close attention to areas frequently exposed to sunlight. They may also ask about the patient’s medical history and risk factors.
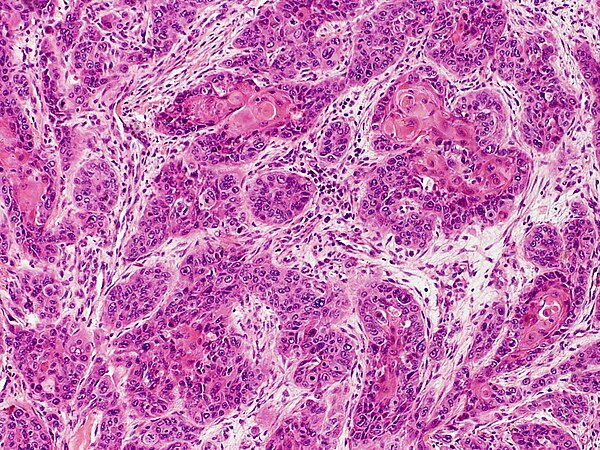
Biopsy
A biopsy is the definitive method for diagnosing squamous cell skin cancer. During this procedure, a small sample of the affected tissue is removed and examined under a microscope. There are several types of biopsies:
- Shave Biopsy: A thin layer of the lesion is shaved off using a surgical blade.
- Punch Biopsy: A circular tool is used to remove a deeper sample of tissue.
- Excisional Biopsy: The entire lesion is surgically removed for analysis.
Imaging Tests
In cases where the cancer has potentially spread beyond the skin, imaging tests such as computed tomography scans, magnetic resonance imaging, or positron emission tomography scans may be ordered. These tests help determine whether the cancer has metastasized to nearby lymph nodes or other organs.
Treatment Options for Squamous Cell Skin Cancer
The treatment approach for squamous cell skin cancer depends on various factors, including the size, location, and stage of the tumor, as well as the patient’s overall health. Early detection often leads to successful outcomes, as localized tumors are easier to treat.
Surgical Removal
Surgery is the most common treatment for squamous cell skin cancer. Several surgical techniques are available:
- Excision Surgery: The cancerous tissue, along with a margin of healthy skin, is cut out to ensure complete removal of the tumor.
- Mohs Surgery: This specialized technique involves removing thin layers of tissue one at a time and examining them under a microscope until no cancer cells remain. It is particularly effective for cancers located in cosmetically sensitive areas, such as the face.
- Curettage and Electrodessication: The tumor is scraped away using a curette, and an electric needle is used to destroy any remaining cancer cells.
Radiation Therapy
Radiation therapy uses high-energy beams to target and destroy cancer cells. It is typically recommended for patients who cannot undergo surgery due to medical reasons or for tumors located in difficult-to-reach areas. Radiation therapy may also be used after surgery to eliminate any residual cancer cells.
Cryotherapy
Cryotherapy involves freezing the cancerous tissue with liquid nitrogen. This method is suitable for small, superficial tumors and is often used when surgery is not an option. The frozen tissue eventually sloughs off, allowing healthy skin to regenerate.
Topical Treatments
For very early-stage squamous cell skin cancer or precancerous lesions, topical medications may be prescribed. These treatments include creams or ointments containing chemotherapy agents or immune response modifiers that work to destroy cancer cells on the surface of the skin.
Photodynamic Therapy
Photodynamic therapy combines a photosensitizing agent with a specific type of light to kill cancer cells. After applying the agent to the affected area, the skin is exposed to light, which activates the medication and destroys the targeted cells. This treatment is minimally invasive and leaves minimal scarring.
Targeted Therapy and Immunotherapy
In advanced cases where squamous cell skin cancer has spread, systemic treatments like targeted therapy and immunotherapy may be employed. Targeted therapy focuses on specific molecular pathways involved in cancer growth, while immunotherapy harnesses the body’s immune system to fight the disease.
Preventive Measures
While not all cases of squamous cell skin cancer can be prevented, adopting certain habits can significantly reduce the risk:
- Avoid excessive sun exposure, especially during peak hours between ten in the morning and four in the afternoon.
- Wear protective clothing, such as wide-brimmed hats and long-sleeved shirts, when outdoors.
- Use broad-spectrum sunscreen with a sun protection factor of at least thirty and reapply every two hours.
- Avoid tanning beds and artificial sources of ultraviolet radiation.
- Perform regular self-examinations of the skin to detect any unusual changes early.