Spondylolisthesis, often abbreviated as “SPL,” is a condition that affects the spine, specifically the vertebrae. It occurs when one of the bones in the spinal column slips out of its normal position and moves forward or backward relative to the bone below it. This slippage can lead to various symptoms, including pain, stiffness, and even nerve compression. Understanding the causes, recognizing the symptoms, obtaining an accurate diagnosis, and exploring treatment options are essential for managing this condition effectively.

What Is Spondylolisthesis?
Spondylolisthesis is derived from two Greek words: “spondylos,” meaning vertebra, and “olisthesis,” meaning to slip. This condition primarily affects the lower back but can also occur in other areas of the spine. The severity of the slippage is graded on a scale from one to five, with grade one being the mildest and grade five indicating complete dislocation of the vertebra.
The condition can develop due to several factors, ranging from congenital issues present at birth to degenerative changes that occur with age. While some individuals may experience no symptoms, others may face debilitating pain and functional limitations. Early identification and appropriate management are crucial to prevent further complications.
Causes of Spondylolisthesis
There are multiple causes of this spinal condition, and understanding these factors can help in both prevention and treatment. Below are the primary causes:
1. Congenital Factors
Congenital spondylolisthesis occurs when there is an abnormal formation of the spine during fetal development. In such cases, the vertebrae may not form correctly, leading to instability and an increased risk of slippage later in life.
2. Degenerative Changes
As people age, the discs and joints in the spine can wear down due to natural degeneration. This process weakens the structures that support the vertebrae, making them more prone to slipping. Degenerative spondylolisthesis is most common in older adults and typically affects the lower back.
3. Trauma or Injury
A sudden injury or trauma to the spine, such as a fracture, can cause one vertebra to slip out of place. This type of spondylolisthesis is referred to as traumatic and is often seen in individuals involved in high-impact sports or accidents.
4. Pathological Conditions
Certain diseases, such as tumors or infections, can weaken the bones and tissues of the spine, leading to slippage. This form of spondylolisthesis is known as pathological and requires addressing the underlying condition to manage the spinal issue effectively.
5. Repetitive Stress
Activities that involve repetitive stress on the spine, such as gymnastics, weightlifting, or football, can increase the risk of developing spondylolisthesis. Over time, the repeated strain can lead to small fractures or weakening of the vertebrae, causing them to slip.
Symptoms of Spondylolisthesis
The symptoms of this condition can vary widely depending on the severity of the slippage and the specific area of the spine affected. Some individuals may remain asymptomatic, while others may experience significant discomfort. Common symptoms include:
- Lower Back Pain: Persistent pain in the lower back is one of the most common symptoms. The pain may worsen with activity and improve with rest.
- Muscle Tightness: Tightness or spasms in the muscles surrounding the affected area are frequently reported.
- Pain Radiating to the Legs: If the slipped vertebra compresses a nerve, it can cause pain, numbness, or tingling that radiates down one or both legs.
- Stiffness: Many individuals experience stiffness in the lower back, which can limit their range of motion.
- Difficulty Walking: Severe cases may lead to difficulty walking or maintaining balance due to nerve involvement.
Diagnosis of Spondylolisthesis
An accurate diagnosis is essential for determining the appropriate treatment plan. Healthcare providers use a combination of methods to diagnose this condition:
1. Medical History and Physical Examination
The diagnostic process begins with a thorough review of the patient’s medical history and a physical examination. During the exam, the healthcare provider will assess the patient’s posture, range of motion, and any signs of muscle weakness or nerve involvement.
2. Imaging Tests
Imaging tests play a critical role in confirming the presence of spondylolisthesis and determining its severity. Common imaging techniques include:
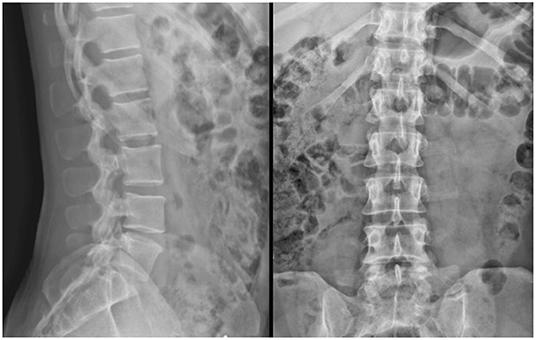
- X-rays: X-rays provide a clear view of the bones in the spine and can reveal whether a vertebra has slipped out of place.
- Magnetic Resonance Imaging (MRI): An MRI offers detailed images of the soft tissues, including the discs, nerves, and ligaments. This test helps identify nerve compression or damage.
- Computed Tomography (CT) Scan: A CT scan provides cross-sectional images of the spine and can help detect fractures or other structural abnormalities.
3. Grading the Severity
Once the condition is confirmed, the degree of slippage is graded using a standardized system. This grading helps guide treatment decisions:
- Grade I: Less than 25 percent slippage
- Grade II: 26 to 50 percent slippage
- Grade III: 51 to 75 percent slippage
- Grade IV: 76 to 99 percent slippage
- Grade V: Complete dislocation of the vertebra
Treatment Options for Spondylolisthesis
The treatment approach for this condition depends on the severity of the slippage, the presence of symptoms, and the impact on daily life. Treatment options range from conservative measures to surgical interventions.
1. Non-Surgical Treatments
For mild to moderate cases, non-surgical treatments are often effective in managing symptoms and improving function. These include:
- Rest and Activity Modification: Avoiding activities that exacerbate symptoms can help reduce pain and allow the spine to heal.
- Physical Therapy: A tailored exercise program can strengthen the muscles supporting the spine, improve flexibility, and enhance overall function.
- Medications: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can alleviate discomfort. In some cases, prescription medications may be necessary.
- Epidural Steroid Injections: These injections deliver anti-inflammatory medication directly to the affected area, providing temporary relief from pain and inflammation.
2. Bracing
In certain cases, particularly among younger patients, a back brace may be recommended to stabilize the spine and prevent further slippage. Bracing is typically used as a short-term solution and is combined with other treatments.
3. Surgical Interventions
Surgery is considered for severe cases or when conservative treatments fail to provide relief. The goal of surgery is to stabilize the spine, relieve nerve compression, and restore proper alignment. Common surgical procedures include:
- Spinal Fusion: This procedure involves fusing two or more vertebrae together to prevent movement and stabilize the spine.
- Laminectomy: A laminectomy removes part of the vertebra to relieve pressure on the nerves.
- Decompression Surgery: This surgery aims to alleviate nerve compression by removing bone or tissue that is pressing on the nerves.
4. Lifestyle Modifications
In addition to medical treatments, making lifestyle changes can significantly improve outcomes. Maintaining a healthy weight, practicing good posture, and avoiding activities that strain the spine can help prevent further complications.
Prevention Strategies
While not all cases of spondylolisthesis can be prevented, certain strategies can reduce the risk of developing this condition:
- Exercise Regularly: Strengthening the core and back muscles through regular exercise can provide better support for the spine.
- Use Proper Lifting Techniques: When lifting heavy objects, bend at the knees and keep the back straight to avoid unnecessary strain.
- Avoid High-Impact Activities: Limit participation in activities that place excessive stress on the spine, especially if you have a history of back problems.