Spina Bifida, often abbreviated as SB, is a congenital condition that affects the development of the spine and spinal cord. It occurs when the neural tube, which eventually forms the brain and spinal cord, does not close properly during early fetal development. This condition can lead to a range of physical and neurological challenges, depending on its severity. In this article, we will explore the causes, types, symptoms, and treatments associated with Spina Bifida to provide a comprehensive understanding of this complex medical condition.
What Causes Spina Bifida?
The exact cause of Spina Bifida remains unclear, but researchers believe it results from a combination of genetic and environmental factors. Below are some of the most commonly identified contributing factors:
Genetic Factors
- Family history plays a significant role in the likelihood of Spina Bifida. If one child in a family is born with the condition, the chances of having another child with it increase.
- Certain genetic mutations or chromosomal abnormalities may predispose an individual to the condition.
Nutritional Deficiencies
- A deficiency in folic acid, a type of vitamin B, during pregnancy is strongly linked to the development of Spina Bifida. Folic acid is essential for proper neural tube closure.
- Poor maternal nutrition or inadequate intake of vitamins and minerals can heighten the risk.
Environmental Influences
- Exposure to certain medications, such as anticonvulsants, during pregnancy may increase the likelihood of Spina Bifida.
- Maternal health conditions like diabetes or obesity have been associated with a higher risk of the condition.
- Excessive alcohol consumption or smoking during pregnancy can also contribute to developmental issues in the fetus.
Other Risk Factors
- Advanced maternal age or a history of miscarriages may elevate the chances of Spina Bifida.
- Living in areas with limited access to healthcare or nutritional resources can exacerbate the risk.
Types of Spina Bifida
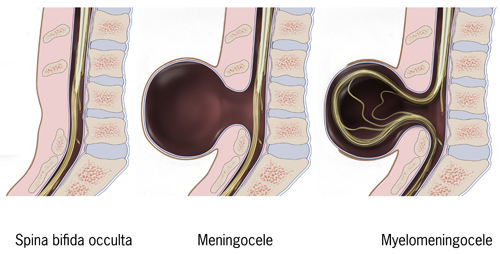
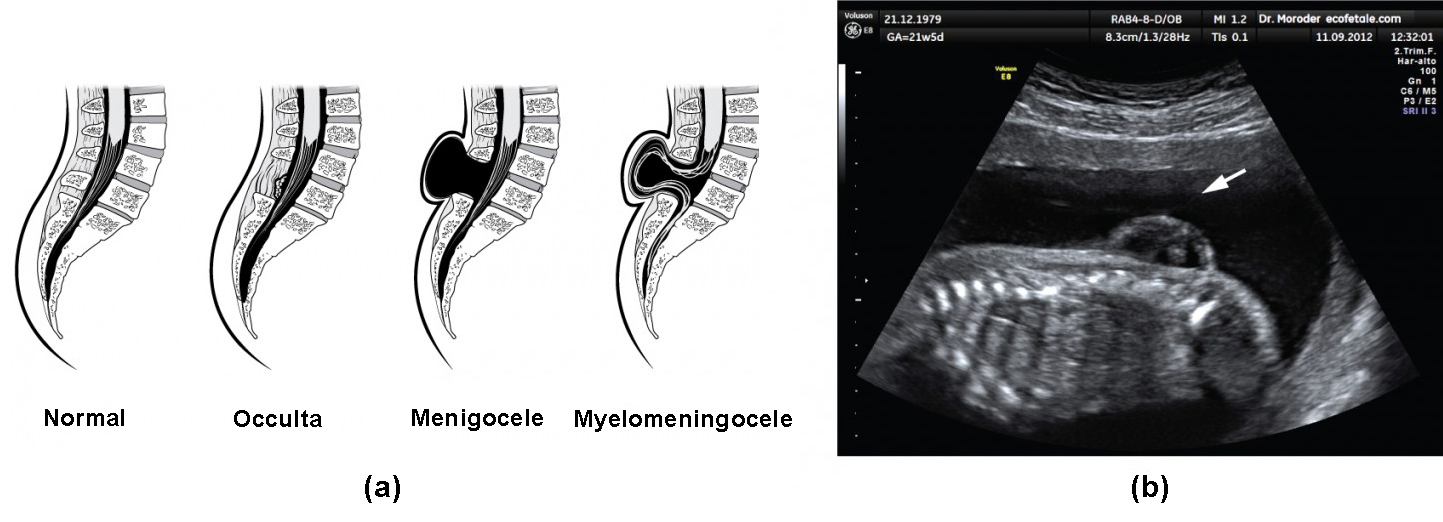
Spina Bifida manifests in several forms, each varying in severity and impact on the individual. The three primary types are described below:
Spina Bifida Occulta
This is the mildest form of the condition and often goes undiagnosed because it typically does not cause noticeable symptoms. In Spina Bifida Occulta, there is a small gap in the vertebrae, but the spinal cord and surrounding tissues remain intact. Many individuals with this type may only discover it incidentally during imaging tests for unrelated issues.
Meningocele
In this type, the protective membranes around the spinal cord, known as the meninges, protrude through an opening in the spine. A sac forms outside the body, but the spinal cord itself remains in place. Meningocele generally causes fewer complications compared to more severe forms, though surgery is often required to correct the defect.
Myelomeningocele
Myelomeningocele is the most severe form of Spina Bifida. In this case, both the meninges and parts of the spinal cord protrude through the opening in the spine, forming a visible sac on the back. This type often leads to significant nerve damage, resulting in paralysis, loss of sensation, and other neurological issues. Individuals with Myelomeningocele may also experience complications such as hydrocephalus, where excess fluid accumulates in the brain.
Symptoms of Spina Bifida
The symptoms of Spina Bifida vary widely depending on the type and severity of the condition. Some individuals may experience mild effects, while others face more profound challenges. Common symptoms include:
Physical Symptoms
- Visible abnormalities on the back, such as a dimple, birthmark, or tuft of hair, particularly in cases of Spina Bifida Occulta.
- A fluid-filled sac or swelling on the back, characteristic of Meningocele or Myelomeningocele.
- Weakness or paralysis in the legs due to nerve damage.
- Deformities in the feet, hips, or spine, such as scoliosis or clubfoot.
Neurological Symptoms
- Loss of sensation in the lower extremities or areas affected by nerve damage.
- Bowel and bladder dysfunction, including incontinence or difficulty controlling these functions.
- Hydrocephalus, which can cause headaches, vomiting, seizures, and developmental delays if left untreated.
Developmental Symptoms
- Delayed milestones in motor skills, such as crawling or walking.
- Learning disabilities or cognitive impairments, particularly in individuals with Myelomeningocele.
- Difficulty with coordination and balance.
Treatment Options for Spina Bifida
While there is no cure for Spina Bifida, various treatments can help manage symptoms and improve quality of life. The approach depends on the type and severity of the condition, as well as the specific needs of the individual.
Surgical Interventions
Surgery is often necessary to address the physical defects caused by Spina Bifida. Common procedures include:
- Repair of the Spinal Defect: In cases of Meningocele or Myelomeningocele, surgery is performed shortly after birth to close the opening in the spine and prevent infection.
- Shunt Placement: For individuals with hydrocephalus, a shunt may be inserted to drain excess fluid from the brain into the abdomen.
- Fetal Surgery: In some cases, surgery can be performed on the fetus while still in the womb to repair the spinal defect before birth. This approach has shown promise in reducing the severity of symptoms.
Physical Therapy and Rehabilitation
Physical therapy plays a crucial role in helping individuals with Spina Bifida achieve greater mobility and independence. Key components include:
- Exercises to strengthen muscles and improve flexibility.
- Use of assistive devices such as braces, crutches, or wheelchairs to aid movement.
- Occupational therapy to develop skills for daily living activities.
Management of Bowel and Bladder Issues
Bowel and bladder dysfunction are common challenges for individuals with Spina Bifida. Treatment options include:
- Catheterization to manage urinary retention or incontinence.
- Dietary modifications and medications to regulate bowel movements.
- Behavioral training to establish routines for managing these functions.
Educational and Psychological Support
Children with Spina Bifida may benefit from specialized educational programs tailored to their learning needs. Additionally, psychological support can help address emotional challenges such as anxiety, depression, or low self-esteem. Family counseling may also be beneficial in helping loved ones cope with the demands of caregiving.
Ongoing Medical Care
Individuals with Spina Bifida require lifelong monitoring and care to address potential complications. Regular check-ups with specialists, such as neurologists, orthopedic surgeons, and urologists, are essential. Vaccinations and preventive measures are also important to reduce the risk of infections, particularly in those with compromised immune systems.
Lifestyle Modifications and Coping Strategies
Beyond medical interventions, lifestyle adjustments can significantly enhance the well-being of individuals with Spina Bifida. These include:
- Maintaining a healthy diet rich in nutrients to support overall health and prevent complications like obesity.
- Engaging in adaptive sports or recreational activities to promote physical fitness and social interaction.
- Building a strong support network of family, friends, and community organizations to foster a sense of belonging.
By combining medical treatments with holistic approaches, individuals with Spina Bifida can lead fulfilling lives despite the challenges posed by the condition.