A spermatocele, also known as a spermatic cyst, is a benign condition that affects the male reproductive system. It involves the formation of a fluid-filled sac within the scrotum, typically located near the testicle. While this condition is not life-threatening, it can cause discomfort or concern for those affected. In this article, we will explore the causes, symptoms, and treatment options available for individuals dealing with this condition.
Understanding Spermatoceles
To fully grasp what a spermatocele is, it is important to understand its anatomical context. The epididymis is a coiled tube located on the back of each testicle. Its primary function is to store and transport sperm. A spermatocele develops when a cyst forms in the epididymis, filling with fluid that may contain dead sperm cells. These cysts are usually small, but in some cases, they can grow large enough to be noticeable or cause discomfort.
How Common Are Spermatoceles?
Spermatoceles are relatively common and are often discovered during routine physical examinations. They tend to occur more frequently in men over the age of 40, though they can develop at any age. Despite their prevalence, many men remain unaware of their existence unless they experience symptoms or complications.
Causes of Spermatoceles
The exact cause of spermatoceles is not fully understood, but several factors may contribute to their development:
Blockage in the Epididymis
- A blockage in the tubes of the epididymis can lead to the accumulation of fluid, which may result in the formation of a cyst. This blockage could be due to inflammation, injury, or an infection in the area.
Trauma or Injury
- Physical trauma to the scrotum or testicles can sometimes trigger the development of a spermatocele. Such injuries may disrupt the normal functioning of the epididymis, leading to cyst formation.
Inflammation
- Inflammatory conditions affecting the reproductive system, such as epididymitis, may increase the likelihood of developing a spermatocele. Chronic inflammation can weaken the walls of the epididymis, making it more susceptible to cyst formation.
Age-Related Changes
- As men age, the tissues in the reproductive system may undergo changes that make them more prone to developing cysts. This is why spermatoceles are more commonly observed in older men.
Symptoms of Spermatoceles
Spermatoceles often do not cause noticeable symptoms, especially when they are small. However, as they grow larger, certain signs may become apparent:
Painless Lump or Swelling
- One of the most common symptoms of a spermatocele is the presence of a painless lump or swelling above or behind the testicle. This lump is typically smooth and can vary in size.
Heaviness or Discomfort
- Some men may experience a feeling of heaviness or discomfort in the affected testicle, particularly if the spermatocele grows large enough to put pressure on surrounding tissues.
Visible Changes in the Scrotum
- In more severe cases, the spermatocele may cause visible changes in the shape or size of the scrotum. This can lead to self-consciousness or anxiety for some individuals.
Rare Symptoms
- While uncommon, some men may experience mild pain or a dull ache in the scrotum. This is usually associated with larger cysts that exert pressure on nearby nerves or structures.
Diagnosing Spermatoceles
If a man suspects he has a spermatocele, it is important to consult a healthcare provider for proper diagnosis. The diagnostic process typically involves the following steps:
Physical Examination
- A doctor will perform a physical examination of the scrotum to assess the size, shape, and location of the lump. They may use a technique called transillumination, where a light is shone through the scrotum to determine whether the lump is filled with fluid or solid tissue.
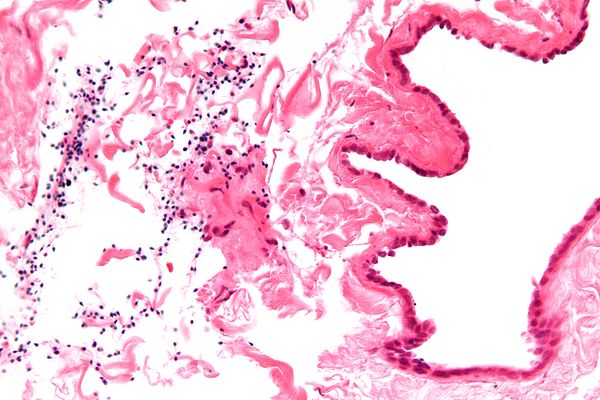
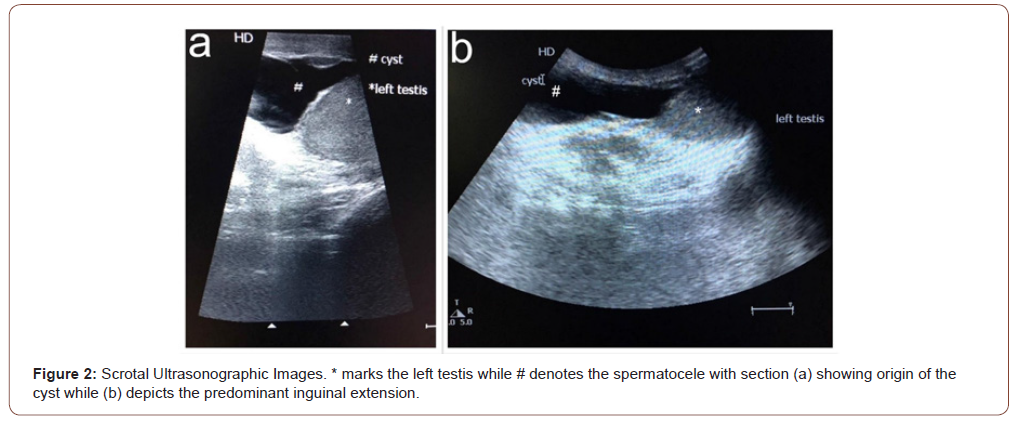
Ultrasound Imaging
- In cases where the diagnosis is unclear, an ultrasound of the scrotum may be recommended. This imaging test provides detailed pictures of the internal structures, helping to confirm the presence of a spermatocele and rule out other conditions, such as tumors or hernias.
Treatment Options for Spermatoceles
Treatment for spermatoceles depends on the severity of symptoms and the impact on the individual’s quality of life. In many cases, no treatment is necessary, but there are options available for those who require intervention.
Observation and Monitoring
- For small, asymptomatic spermatoceles, doctors often recommend a “watch and wait” approach. Regular monitoring ensures that the cyst does not grow or cause complications over time.
Medications
- While medications cannot eliminate a spermatocele, over-the-counter pain relievers such as ibuprofen or acetaminophen may help alleviate discomfort or pain associated with the condition.
Aspiration
- In some cases, a doctor may use a needle to drain the fluid from the cyst. This procedure, known as aspiration, provides temporary relief but carries a risk of recurrence or infection.
Surgical Removal
- For larger or symptomatic spermatoceles, surgery may be recommended. The most common procedure is called a spermatocelectomy, which involves removing the cyst while preserving the epididymis and testicle. This outpatient surgery is typically performed under local or general anesthesia and has a high success rate.
Lifestyle Adjustments
- Men with spermatoceles may benefit from wearing supportive underwear or a jockstrap to reduce discomfort and prevent further irritation. Avoiding activities that strain the groin area can also help manage symptoms.
Potential Complications of Spermatoceles
While spermatoceles are generally harmless, there are a few potential complications to be aware of:
Infection
- Although rare, a spermatocele can become infected, leading to symptoms such as redness, warmth, and increased pain in the scrotum. Prompt medical attention is necessary to address infections effectively.
Recurrence After Treatment
- Even after surgical removal, there is a small chance that a spermatocele may return. Regular follow-up appointments with a healthcare provider can help monitor for recurrence.
Impact on Fertility
- In most cases, spermatoceles do not affect fertility. However, if the cyst is large or located in a critical area of the epididymis, it may interfere with sperm transport. Men concerned about fertility should discuss their concerns with a specialist.
Preventing Spermatoceles
Since the exact cause of spermatoceles is not well understood, there are no guaranteed methods for prevention. However, adopting certain habits may reduce the risk of developing this condition:
- Protecting the groin area from injury by wearing protective gear during sports or physical activities.
- Seeking prompt treatment for infections or inflammatory conditions affecting the reproductive system.
- Maintaining overall reproductive health through regular check-ups and a healthy lifestyle.
When to Seek Medical Attention
It is important to consult a healthcare provider if you notice any unusual changes in the scrotum, such as lumps, swelling, or pain. While spermatoceles are typically benign, these symptoms could also indicate more serious conditions, such as testicular cancer or a hernia. Early diagnosis and treatment are key to ensuring optimal outcomes.