A seroma is a condition that occurs when clear fluid accumulates under the surface of the skin. It is often abbreviated as SE in medical contexts but for the purpose of this article, we will refer to it by its full name. Seromas are commonly seen after surgical procedures or injuries, and while they are generally harmless, they can sometimes lead to complications if left untreated. Understanding what causes a seroma, recognizing its symptoms, and knowing how to manage it are essential for ensuring proper recovery. This article will explore these aspects in detail.
What Is a Seroma?
A seroma is a pocket of clear fluid that forms under the skin. This fluid is similar to the fluid found in blisters and is made up of blood plasma, lymphatic fluid, and other components. While seromas are most commonly associated with surgical procedures, they can also develop after trauma or injury to the body. The fluid accumulation occurs because the body’s natural healing process involves the movement of fluids to the affected area to aid in tissue repair. However, when too much fluid gathers and does not get reabsorbed by the body, it forms a seroma.
Seromas are typically soft to the touch and may feel like a swollen or squishy lump beneath the skin. They are usually painless but can cause discomfort depending on their size and location. In some cases, seromas can become infected, leading to more serious complications.
Common Causes of Seromas
Seromas can develop for various reasons, but they are most frequently linked to surgical procedures. Below are some common causes:
Surgical Procedures
- Major Surgeries: Surgeries that involve large incisions, such as mastectomies, abdominoplasties (tummy tucks), or lymph node removal, are more likely to result in seromas. This is because these procedures disrupt the body’s natural drainage pathways.
- Minimally Invasive Surgeries: Even less invasive surgeries, such as laparoscopic procedures, can sometimes lead to seromas, although the risk is lower compared to open surgeries.
Trauma or Injury
- Blunt Force Trauma: A significant impact to the body, such as from a car accident or fall, can damage tissues and lead to fluid accumulation.
- Burns: Severe burns can cause the body to produce excess fluid as part of the healing process, increasing the likelihood of seroma formation.
Underlying Medical Conditions
- Lymphedema: This condition, which involves the buildup of lymphatic fluid, can predispose individuals to seromas due to impaired drainage.
- Infections: Certain infections can trigger an inflammatory response that leads to fluid accumulation.
Symptoms of a Seroma
Identifying a seroma early can help prevent complications and ensure timely treatment. The following are common symptoms associated with seromas:
Physical Characteristics
- Swelling: A noticeable bulge or lump under the skin is one of the primary signs of a seroma. The swelling may increase over time if the fluid continues to accumulate.
- Soft Texture: Unlike solid masses, seromas tend to feel soft or squishy when touched.
- Discoloration: The skin over the seroma may appear slightly discolored or bruised, especially if the seroma developed after surgery or trauma.
Associated Symptoms
- Pain or Discomfort: While many seromas are painless, larger ones can press on surrounding tissues, causing discomfort or a feeling of heaviness.
- Redness and Warmth: If the seroma becomes infected, the area may become red, warm to the touch, and tender.
- Fever: In cases of infection, individuals may experience fever or chills, indicating a more serious issue that requires immediate medical attention.
Risk Factors for Developing a Seroma
Certain factors can increase the likelihood of developing a seroma. Understanding these risk factors can help individuals take preventive measures and seek appropriate care if necessary.
Surgical Factors
- Extent of Tissue Removal: Procedures that involve the removal of large amounts of tissue or fat are more likely to result in seromas.
- Drainage Systems: The absence or improper use of surgical drains can contribute to fluid buildup.
Individual Factors
- Age: Older adults may be at a higher risk due to slower healing processes.
- Obesity: Excess body weight can put additional pressure on tissues, increasing the risk of fluid accumulation.
- Previous History: Individuals who have experienced seromas in the past are more likely to develop them again.
Management Options for Seromas
The management of a seroma depends on its size, location, and whether it is causing any complications. Below are some common approaches used to address seromas:
Observation and Monitoring
For small, asymptomatic seromas, healthcare providers may recommend simply monitoring the condition. Over time, the body may naturally reabsorb the fluid, and the seroma will resolve on its own. During this period, patients are advised to avoid activities that could irritate the area or cause further fluid accumulation.
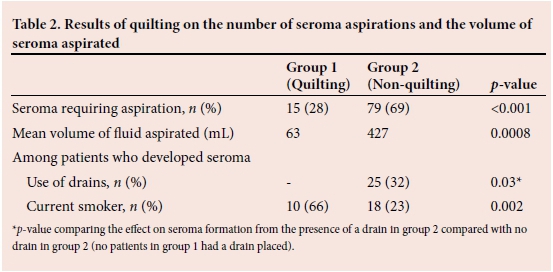
Aspiration
If the seroma is large or causing discomfort, a healthcare provider may perform aspiration. This procedure involves inserting a needle into the seroma to drain the fluid. Aspiration is typically done in a clinical setting to minimize the risk of infection. However, there is a possibility that the seroma may refill with fluid after aspiration, requiring repeated treatments.
Compression Garments
Wearing compression garments can help reduce the size of a seroma by applying gentle pressure to the affected area. This prevents further fluid accumulation and encourages the body to reabsorb the existing fluid. Compression garments are often recommended after surgeries like abdominoplasties or mastectomies to aid in recovery.
Surgical Intervention
In rare cases where a seroma persists despite other treatments, surgical intervention may be necessary. This involves making a small incision to remove the lining of the seroma, known as the capsule, which prevents the fluid from reaccumulating. Surgery is typically considered a last resort due to the risks associated with additional procedures.
Antibiotics
If a seroma becomes infected, antibiotics may be prescribed to treat the infection. It is important to address infections promptly to prevent further complications, such as abscess formation or systemic illness.
Preventive Measures
While not all seromas can be prevented, certain steps can reduce the risk of their development:
- Proper Surgical Technique: Surgeons can minimize the risk of seromas by using meticulous techniques and placing surgical drains when necessary.
- Postoperative Care: Following surgery, adhering to activity restrictions and wearing compression garments as instructed can help prevent fluid buildup.
- Healthy Lifestyle: Maintaining a healthy weight and managing underlying medical conditions can improve overall healing and reduce the likelihood of complications.
When to Seek Medical Attention
While many seromas resolve on their own, certain signs indicate the need for medical evaluation:
- Rapid Growth: If the seroma grows significantly in a short period, it may require drainage or further investigation.
- Persistent Pain: Pain that worsens or does not improve with time should be assessed by a healthcare provider.
- Signs of Infection: Redness, warmth, pus, or fever are warning signs of infection that necessitate immediate medical attention.