Septic shock, often abbreviated as SS, is a life-threatening condition that arises when an infection leads to dangerously low blood pressure and organ dysfunction. It represents the most severe form of sepsis and requires immediate medical attention. This guide aims to provide a detailed understanding of septic shock, including its causes, symptoms, and available treatments.
What is Septic Shock?
Septic shock occurs when the body’s response to an infection spirals out of control, leading to widespread inflammation and damage to tissues and organs. Unlike milder forms of sepsis, septic shock is characterized by a significant drop in blood pressure that does not respond adequately to fluid resuscitation. This can result in insufficient blood flow to vital organs, causing them to fail.
How Does Septic Shock Differ from Sepsis?
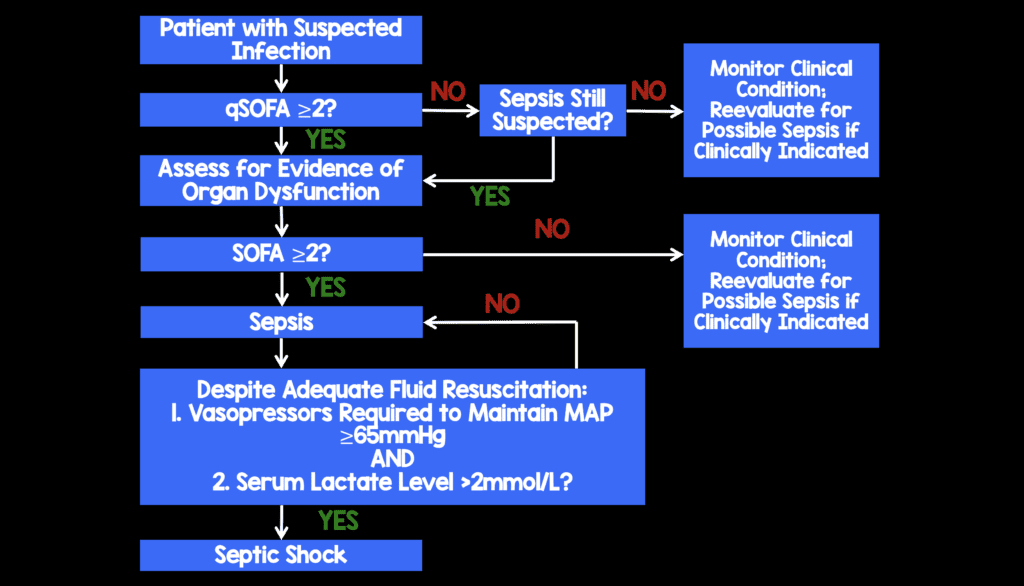
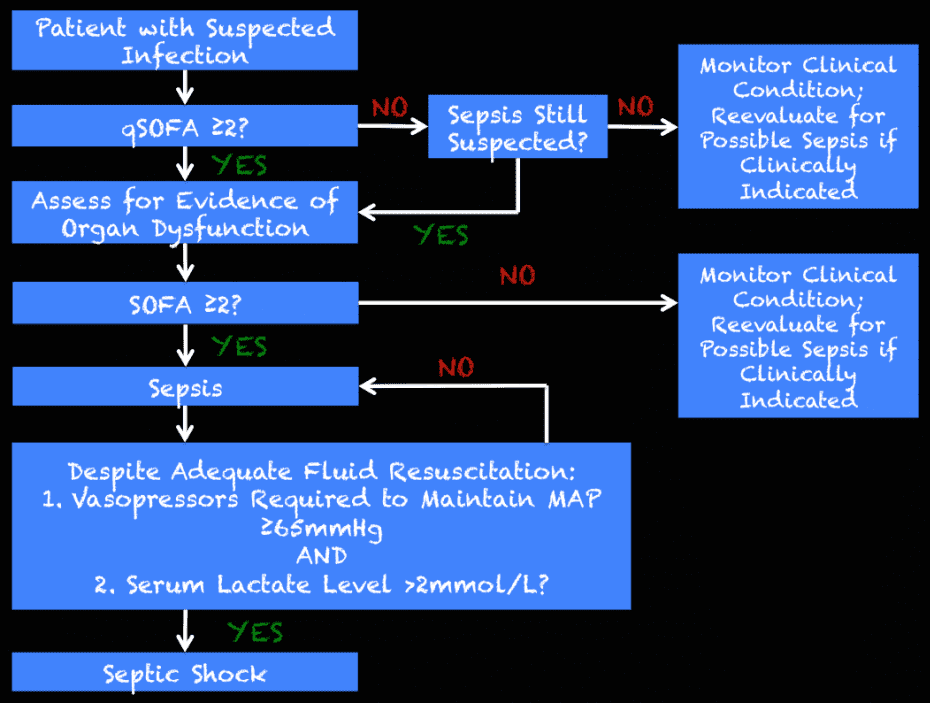
- Sepsis: A systemic inflammatory response to an infection that may cause organ dysfunction but does not necessarily involve severe hypotension.
- Septic Shock: A more advanced stage of sepsis where persistent low blood pressure and organ failure occur despite efforts to stabilize the patient with fluids.
Causes of Septic Shock
Septic shock typically begins with an infection, which can originate from various sources in the body. Understanding these sources is crucial for early identification and treatment.
Common Infection Sources
- Lung Infections: Pneumonia is one of the most frequent causes of septic shock. Bacteria, viruses, or fungi infect the lungs, leading to systemic complications.
- Urinary Tract Infections: These infections, especially when untreated, can spread to the kidneys and bloodstream, triggering a severe immune response.
- Abdominal Infections: Conditions like appendicitis, peritonitis, or infections of the gallbladder can lead to septic shock if they are not promptly addressed.
- Bloodstream Infections: Also known as bacteremia, these infections occur when bacteria or other pathogens enter the bloodstream directly.
- Skin and Soft Tissue Infections: Severe wounds, burns, or abscesses can serve as entry points for pathogens that may cause septic shock.
Risk Factors for Developing Septic Shock
Certain individuals are at a higher risk of developing septic shock due to underlying health conditions or circumstances. These include:
- People with weakened immune systems, such as those undergoing chemotherapy or living with HIV/AIDS.
- Individuals with chronic illnesses like diabetes, kidney disease, or liver disease.
- Elderly patients, whose immune systems may be less effective at fighting infections.
- Patients who have recently undergone surgery or invasive medical procedures.
- Those using medical devices like catheters or ventilators, which can introduce pathogens into the body.
Symptoms of Septic Shock
Recognizing the symptoms of septic shock early can significantly improve outcomes. The signs and symptoms often develop rapidly and can vary depending on the severity of the condition.
Early Warning Signs
- Fever or abnormally low body temperature.
- Rapid heart rate.
- Rapid breathing or shortness of breath.
- Confusion or disorientation.
- Extreme fatigue or weakness.
Advanced Symptoms
As septic shock progresses, the following symptoms may appear:
- Severely low blood pressure that does not improve with fluid administration.
- Reduced urine output due to impaired kidney function.
- Cool, clammy skin or a bluish tint to the skin.
- Difficulty breathing or rapid, shallow breathing.
- Unresponsiveness or loss of consciousness.
Organ-Specific Symptoms
Septic shock can affect multiple organs, leading to specific symptoms based on the organ involved:
- Kidneys: Decreased urine production, swelling in the legs or ankles.
- Lungs: Severe difficulty breathing, chest pain, or coughing up blood.
- Heart: Irregular heartbeat, chest pain, or palpitations.
- Brain: Confusion, agitation, seizures, or coma.
Treatment Options for Septic Shock
Septic shock is a medical emergency that requires immediate intervention. Treatment focuses on stabilizing the patient, controlling the infection, and supporting failing organs.
Initial Stabilization
The first step in treating septic shock is stabilizing the patient’s condition. This includes:
- Administering intravenous fluids to increase blood pressure and improve circulation.
- Providing oxygen therapy to ensure adequate oxygen delivery to tissues.
- Monitoring vital signs closely to assess the patient’s response to treatment.
Infection Control
Identifying and addressing the source of infection is critical to managing septic shock. This may involve:
- Performing blood tests, imaging studies, or cultures to pinpoint the causative organism.
- Administering broad-spectrum antibiotics immediately, even before the exact pathogen is identified.
- Adjusting antibiotic therapy once the specific organism is known to ensure targeted treatment.
- Draining abscesses or removing infected tissues surgically, if necessary.
Supportive Care
Supportive care is essential to help the body recover while the infection is being treated. This includes:
- Using medications like vasopressors to maintain blood pressure if fluids alone are insufficient.
- Providing mechanical ventilation if the patient has difficulty breathing.
- Administering medications to manage complications like blood clots or gastrointestinal bleeding.
- Offering nutritional support through feeding tubes or intravenous nutrition if the patient cannot eat.
Long-Term Management
Even after the acute phase of septic shock is managed, patients may require ongoing care to address lingering effects. This can include:
- Physical therapy to regain strength and mobility.
- Occupational therapy to assist with daily activities.
- Mental health support to cope with the emotional impact of the illness.
- Regular follow-up appointments to monitor recovery and prevent recurrence.
Preventing Septic Shock
While not all cases of septic shock can be prevented, certain measures can reduce the risk of developing this condition:
- Vaccinating against common infections like pneumonia and influenza.
- Practicing good hygiene, such as regular handwashing, to prevent infections.
- Seeking prompt medical attention for infections, especially if they worsen or do not improve with treatment.
- Managing chronic conditions like diabetes or kidney disease effectively to minimize complications.
- Following post-surgical care instructions carefully to avoid wound infections.
Role of Healthcare Providers
Healthcare providers play a crucial role in preventing septic shock by:
- Screening high-risk patients for early signs of infection.
- Administering prophylactic antibiotics before surgeries when appropriate.
- Educating patients about recognizing symptoms of sepsis and seeking timely care.
- Implementing strict infection control protocols in hospitals and clinics.
Living with the Aftermath of Septic Shock
Survivors of septic shock often face long-term challenges, including physical, cognitive, and emotional effects. Understanding these potential outcomes can help patients and their families prepare for the recovery journey.
Physical Effects
Some common physical effects experienced by survivors include:
- Chronic fatigue and muscle weakness.
- Decreased exercise tolerance and endurance.
- Persistent pain or discomfort in affected areas.
Cognitive and Emotional Challenges
Many survivors report difficulties with memory, concentration, and decision-making. Emotional challenges may include:
- Anxiety and depression.
- Post-traumatic stress disorder related to the experience of critical illness.
- Feelings of isolation or frustration during recovery.
Building a Support Network
Having a strong support network is vital for recovery. This can include:
- Family members and friends who provide emotional and practical support.
- Support groups for sepsis survivors to share experiences and coping strategies.
- Healthcare professionals who offer guidance and encouragement throughout the recovery process.