Sepsis, often abbreviated as SIRS (Systemic Inflammatory Response Syndrome) in medical contexts, is a life-threatening condition that arises when the body’s response to an infection spirals out of control. It is not an infection itself but rather the body’s overwhelming and dysregulated reaction to an infectious agent. This extreme response can lead to widespread inflammation, organ dysfunction, and even death if not treated promptly. In this article, we will explore what sepsis is, how it develops, its symptoms, risk factors, and available treatments.

What Is Sepsis?
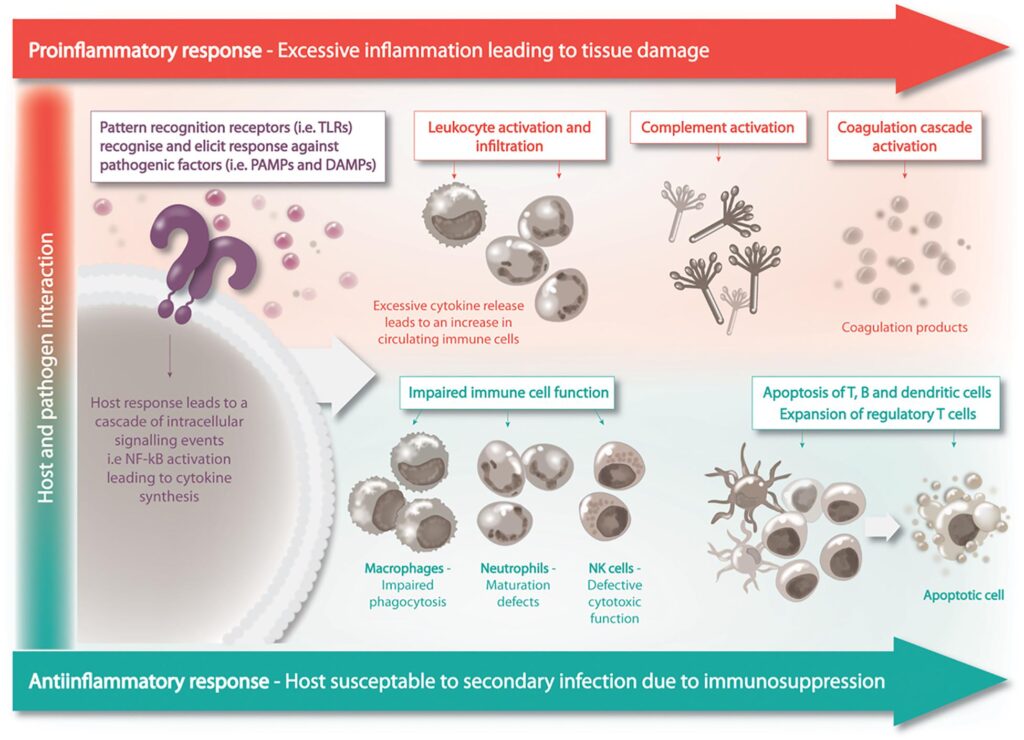
Sepsis occurs when the immune system, which normally fights off infections, goes into overdrive. Instead of targeting only the harmful bacteria, virus, or fungus causing the infection, the immune system begins attacking the body’s own tissues and organs. This cascade of events can result in severe damage to multiple organ systems, including the lungs, kidneys, liver, and heart.
The process starts with an infection, which could be something as common as pneumonia, a urinary tract infection, or a skin infection. When the immune system detects the presence of harmful pathogens, it releases chemicals to combat them. However, in cases of sepsis, these chemicals trigger widespread inflammation throughout the body. This inflammation can cause blood vessels to leak, leading to a dangerous drop in blood pressure and impaired blood flow to vital organs.
How Does Sepsis Develop?
The development of sepsis involves several stages, each progressively more severe:
- Infection: The process begins with an infection caused by bacteria, viruses, fungi, or parasites. Common sources include lung infections, urinary tract infections, abdominal infections, and skin wounds.
- Immune Response Activation: The immune system responds to the infection by releasing chemicals to fight the invading pathogens. These chemicals are meant to contain the infection but sometimes go awry.
- Systemic Inflammation: Instead of localizing the response to the site of infection, the immune system triggers inflammation throughout the body. This systemic inflammation can harm healthy tissues and disrupt normal bodily functions.
- Organ Dysfunction: As inflammation spreads, it can impair the function of vital organs. For example, the lungs may struggle to deliver oxygen, the kidneys may fail to filter waste, and the heart may have difficulty maintaining adequate blood pressure.
- Septic Shock: In the most severe cases, sepsis progresses to septic shock, where blood pressure drops dangerously low, and organs begin to shut down. Without immediate intervention, this stage is often fatal.
Recognizing the Symptoms of Sepsis
One of the challenges of sepsis is that its symptoms can mimic those of other conditions, making it difficult to diagnose early. However, recognizing the signs and seeking prompt medical attention is critical for survival. Symptoms may vary depending on the severity of the condition but generally include:
- High fever or abnormally low body temperature
- Rapid heart rate
- Rapid breathing or shortness of breath
- Confusion or disorientation
- Extreme pain or discomfort
- Cold, clammy, or pale skin
- Reduced urine output
- Nausea or vomiting
In children, additional symptoms may include lethargy, irritability, and refusal to eat or drink. Parents and caregivers should be particularly vigilant if a child has a known infection and begins exhibiting these signs.
When to Seek Medical Attention
Sepsis is a medical emergency, and time is of the essence. If you or someone you know exhibits any combination of the above symptoms, especially in the presence of a known infection, seek medical help immediately. Early recognition and treatment can mean the difference between recovery and severe complications.
Risk Factors for Developing Sepsis
While anyone can develop sepsis, certain individuals are at higher risk due to underlying health conditions, age, or lifestyle factors. Understanding these risk factors can help individuals and healthcare providers take preventive measures. Some common risk factors include:
- Weakened Immune System: People with conditions such as cancer, diabetes, or HIV/AIDS, as well as those taking immunosuppressive medications, are more susceptible to infections and sepsis.
- Chronic Illnesses: Conditions like chronic kidney disease, liver disease, and heart failure increase the risk of developing sepsis.
- Age: Infants, young children, and older adults are more vulnerable due to weaker immune systems or age-related health issues.
- Recent Hospitalization or Surgery: Individuals who have recently undergone surgery, been hospitalized, or had invasive medical procedures are at higher risk of acquiring infections that could lead to sepsis.
- Severe Burns or Wounds: Large burns or open wounds provide entry points for pathogens, increasing the likelihood of infection and sepsis.
- Pregnancy and Childbirth: Complications during pregnancy, childbirth, or postpartum recovery can predispose women to infections that may progress to sepsis.
Preventing Sepsis
While not all cases of sepsis can be prevented, certain measures can significantly reduce the risk:
- Vaccination: Staying up-to-date with vaccinations can prevent many infections that might lead to sepsis.
- Proper Wound Care: Cleaning and dressing cuts, scrapes, and surgical wounds properly can reduce the risk of infection.
- Good Hygiene Practices: Regular handwashing and avoiding contact with sick individuals can help prevent the spread of infections.
- Managing Chronic Conditions: Keeping chronic illnesses under control through medication, diet, and regular check-ups can lower the risk of complications.
- Early Treatment of Infections: Promptly addressing infections, no matter how minor they seem, can prevent them from escalating into sepsis.
Treatment Options for Sepsis
Treating sepsis requires immediate and aggressive medical intervention. The primary goals of treatment are to eliminate the source of infection, stabilize the patient’s condition, and support failing organs. The specific approach depends on the severity of the condition and the organs affected.
Antibiotics and Antimicrobial Therapy
Since most cases of sepsis are caused by bacterial infections, antibiotics are a cornerstone of treatment. Broad-spectrum antibiotics are typically administered intravenously as soon as possible to target a wide range of potential pathogens. Once blood cultures identify the specific bacteria causing the infection, doctors may adjust the antibiotic regimen accordingly.
For viral or fungal infections, antiviral or antifungal medications may be prescribed instead. It is crucial to start antimicrobial therapy as early as possible to improve outcomes.
Fluid Resuscitation
Sepsis often leads to dangerously low blood pressure, a condition known as hypotension. To counteract this, healthcare providers administer intravenous fluids to restore blood volume and improve circulation. Fluid resuscitation helps ensure that vital organs receive adequate oxygen and nutrients.
Vasopressors
In cases where fluid resuscitation alone cannot stabilize blood pressure, medications called vasopressors may be used. These drugs constrict blood vessels and raise blood pressure, helping to maintain adequate blood flow to the organs.
Supportive Care
Patients with severe sepsis or septic shock often require intensive care to support failing organs. This may include:
- Mechanical ventilation to assist with breathing
- Dialysis to support kidney function
- Oxygen therapy to ensure sufficient oxygen levels in the blood
- Medications to manage pain, reduce inflammation, or prevent blood clots
Surgical Intervention
In some cases, the source of the infection may need to be removed surgically. For example, abscesses may require drainage, or infected tissues may need to be debrided or removed entirely. Addressing the root cause of the infection is essential for successful treatment.
Living with the Aftereffects of Sepsis
Surviving sepsis can be a life-changing experience. Many individuals face long-term physical, cognitive, and emotional challenges after recovering from the condition. These aftereffects, collectively referred to as Post-Sepsis Syndrome, can include:
- Fatigue and weakness
- Memory problems and difficulty concentrating
- Muscle and joint pain
- Depression, anxiety, or post-traumatic stress disorder
- Decreased quality of life due to lingering health issues
Rehabilitation programs, counseling, and ongoing medical care can help survivors regain their strength and adapt to life after sepsis.