Seborrheic dermatitis, commonly referred to as SD, is a chronic inflammatory skin condition that affects millions of people worldwide. It primarily targets areas of the body rich in oil-producing glands, such as the scalp, face, and upper chest. While it is not contagious or life-threatening, seborrheic dermatitis can significantly impact an individual’s quality of life due to its visible symptoms and recurring nature. Understanding its causes, recognizing its symptoms, and exploring effective treatments are essential steps toward managing this condition.
What is Seborrheic Dermatitis?
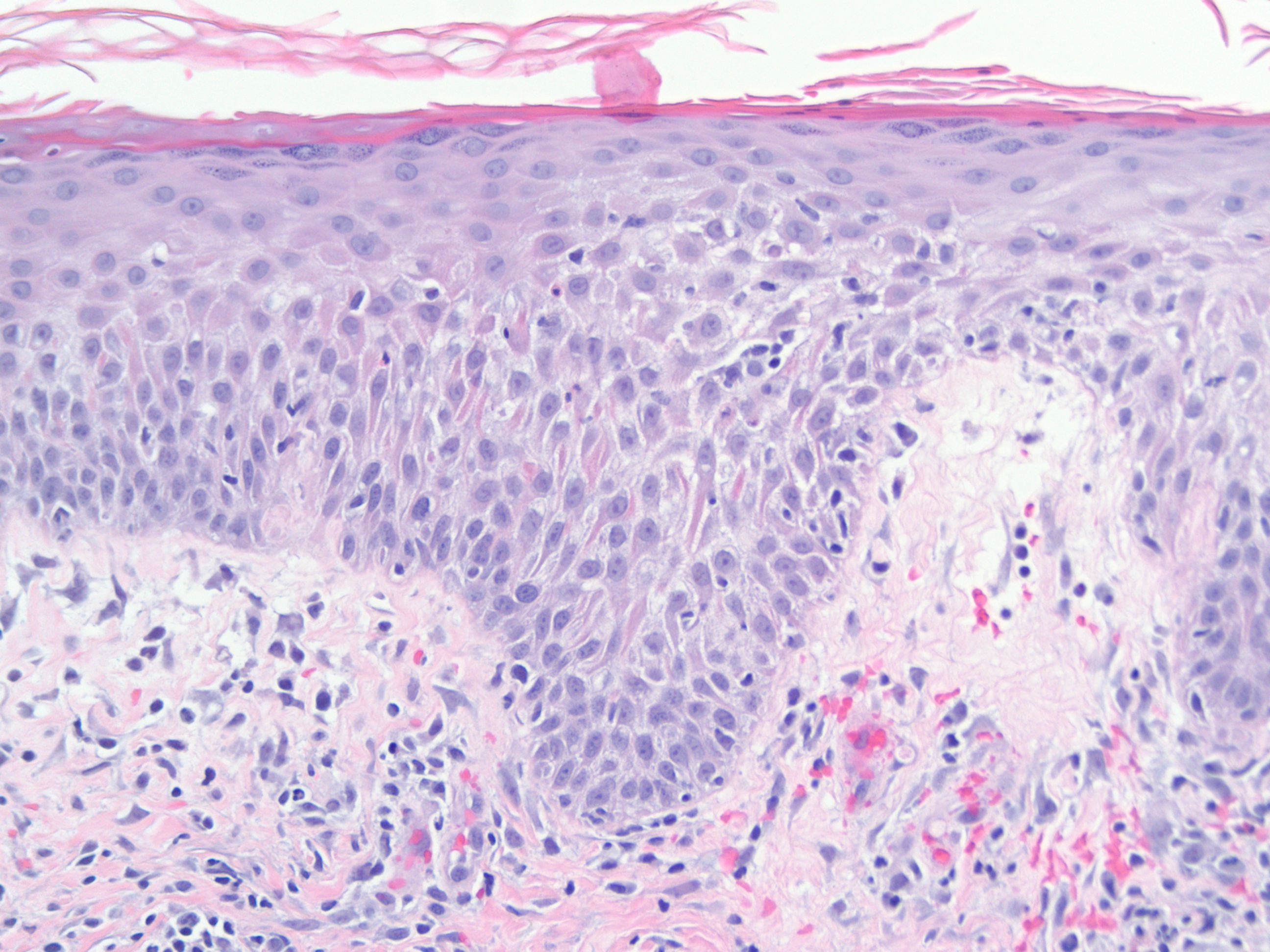
Seborrheic dermatitis is a common skin disorder characterized by red, inflamed, and flaky patches on the skin. These patches often appear greasy and may be accompanied by itching or discomfort. The condition tends to flare up during certain seasons, particularly in cold and dry weather, and can affect individuals of all ages, from infants to adults. In infants, it is often referred to as “cradle cap,” while in adults, it is more commonly associated with dandruff.
Key Features of Seborrheic Dermatitis
- Persistent redness and inflammation
- Oily, yellowish scales or flakes
- Itching or burning sensation in affected areas
- Commonly occurs on the scalp, eyebrows, ears, and nose
Causes of Seborrheic Dermatitis
The exact cause of seborrheic dermatitis remains unclear, but several contributing factors have been identified. These include genetic predisposition, environmental triggers, and interactions with microorganisms living on the skin.
Role of Malassezia Yeast
One of the primary suspects in the development of seborrheic dermatitis is a type of yeast called Malassezia. This yeast naturally resides on the skin’s surface and is generally harmless. However, in individuals prone to seborrheic dermatitis, an overgrowth of Malassezia can trigger an inflammatory response. This leads to increased skin cell turnover, resulting in the characteristic flakiness and redness.
Hormonal and Immune System Factors
Hormonal fluctuations and immune system activity also play a significant role in the onset of seborrheic dermatitis. For instance, stress and fatigue can weaken the immune system, making the skin more susceptible to inflammation. Additionally, hormonal changes during puberty or pregnancy may exacerbate the condition by increasing oil production in the skin.
Environmental and Lifestyle Triggers
Certain environmental factors can worsen seborrheic dermatitis. Cold, dry climates tend to dry out the skin, while humid conditions can increase oil production. Harsh skincare products, excessive washing, and poor hygiene practices may also irritate the skin and trigger flare-ups. Furthermore, lifestyle habits such as smoking and alcohol consumption have been linked to an increased risk of developing the condition.
Symptoms of Seborrheic Dermatitis
The symptoms of seborrheic dermatitis can vary depending on the affected area and the severity of the condition. While some individuals experience mild flakiness, others may suffer from intense redness and irritation.
Common Symptoms
- Red, inflamed patches on the skin
- White or yellowish scales or flakes
- Greasy appearance of the affected areas
- Itching or burning sensation
- Swelling or crusting in severe cases
Symptoms by Location
Seborrheic dermatitis most commonly affects the following areas:
- Scalp: Flaky, white or yellow scales, often mistaken for dandruff
- Face: Redness and scaling around the eyebrows, nose, and ears
- Upper Chest and Back: Greasy, scaly patches that may itch
- Eyelids: Swelling and redness, known as blepharitis
Treatments for Seborrheic Dermatitis
While there is no permanent cure for seborrheic dermatitis, various treatments can help manage symptoms and reduce flare-ups. These treatments range from over-the-counter remedies to prescription medications, depending on the severity of the condition.
Topical Antifungal Treatments
Antifungal creams, shampoos, and lotions are often the first line of defense against seborrheic dermatitis. These products work by targeting the Malassezia yeast, reducing its population on the skin. Common antifungal agents include ketoconazole, ciclopirox, and selenium sulfide. Regular use of these treatments can help control flakiness and inflammation.
Medicated Shampoos
For individuals with scalp involvement, medicated shampoos are highly effective. Ingredients such as zinc pyrithione, salicylic acid, and coal tar can help remove excess oil and dead skin cells. Using these shampoos two to three times a week can significantly improve symptoms.
Topical Corticosteroids
In cases of severe inflammation, topical corticosteroids may be prescribed. These medications reduce redness and swelling by suppressing the immune response. However, prolonged use of corticosteroids can lead to side effects such as thinning of the skin, so they should only be used under medical supervision.
Non-Steroidal Anti-Inflammatory Creams
For those who cannot use corticosteroids, non-steroidal anti-inflammatory creams such as pimecrolimus and tacrolimus offer an alternative. These medications modulate the immune system and reduce inflammation without the risks associated with long-term steroid use.
Lifestyle and Home Remedies
In addition to medical treatments, certain lifestyle changes and home remedies can help alleviate symptoms:
- Maintain Good Hygiene: Wash affected areas regularly with gentle cleansers to prevent oil buildup.
- Avoid Irritants: Steer clear of harsh soaps, detergents, and skincare products that contain alcohol or fragrances.
- Moisturize: Use non-comedogenic moisturizers to keep the skin hydrated without clogging pores.
- Manage Stress: Practice relaxation techniques such as yoga or meditation to reduce stress levels.
- Dietary Adjustments: Some individuals find relief by incorporating anti-inflammatory foods like omega-3 fatty acids into their diet.
When to See a Doctor
While mild cases of seborrheic dermatitis can often be managed at home, it is important to seek medical advice if symptoms persist or worsen. A healthcare provider can rule out other skin conditions, such as psoriasis or eczema, and recommend appropriate treatments. Signs that warrant a visit to the doctor include:
- Severe redness or swelling
- Persistent itching or discomfort
- Signs of infection, such as pus or fever
- No improvement after using over-the-counter treatments
Preventing Flare-Ups
Although seborrheic dermatitis is a chronic condition, taking preventive measures can minimize the frequency and severity of flare-ups. Consistent skincare routines, avoiding known triggers, and maintaining overall health are key strategies for long-term management.
Tips for Prevention
- Use gentle, fragrance-free skincare products
- Avoid excessive heat and humidity
- Wear loose-fitting clothing to prevent irritation
- Stay hydrated and maintain a balanced diet
- Follow a regular treatment regimen as advised by a healthcare provider





