Scleroderma, also known as systemic sclerosis (SSc), is a rare and chronic autoimmune disease that affects the skin and internal organs. This condition leads to the hardening and tightening of the skin and connective tissues, causing significant discomfort and complications for those affected. Understanding scleroderma is crucial for early diagnosis and effective management of its symptoms. In this article, we will explore what scleroderma is, its causes, symptoms, and available treatment options.
What Is Scleroderma?
Scleroderma is a complex disorder characterized by an overproduction of collagen, a protein that provides structure to the skin and other tissues. The excessive buildup of collagen results in thickened, hardened skin and can also affect blood vessels, muscles, and internal organs such as the heart, lungs, kidneys, and digestive system. There are two main types of scleroderma: localized and systemic. Localized scleroderma primarily affects the skin, while systemic scleroderma can impact multiple organs and systems within the body.
Localized Scleroderma
- Morphea: This form causes patches of hardened skin that may be oval-shaped or linear. Morphea typically does not affect internal organs.
- Linear Scleroderma: This type appears as streaks or bands of thickened skin, often on the arms, legs, or forehead. It can sometimes affect underlying muscles and bones.
Systemic Scleroderma
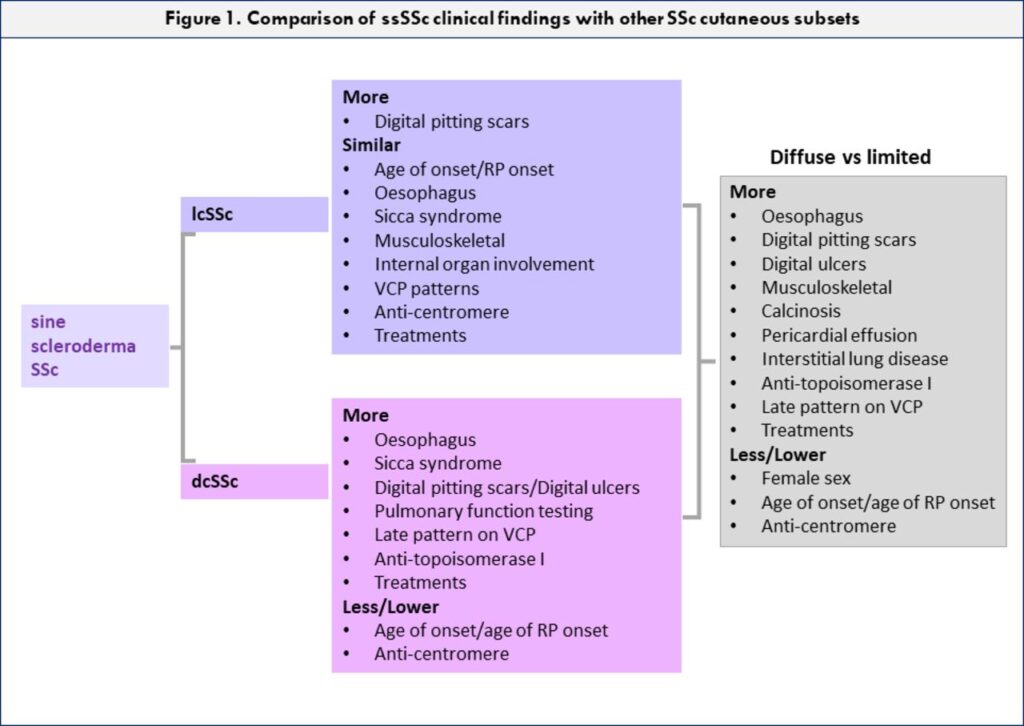
- Limited Cutaneous Systemic Sclerosis: Also known as CREST syndrome, this form progresses slowly and primarily affects the skin of the fingers, hands, face, and lower arms and legs. Internal organ involvement is less severe compared to other forms.
- Diffuse Cutaneous Systemic Sclerosis: This type involves widespread skin thickening and can rapidly progress to affect major organs like the heart, lungs, and kidneys.
Causes of Scleroderma
The exact cause of scleroderma remains unknown, but researchers believe it arises from a combination of genetic and environmental factors. Here are some key contributors:
Autoimmune Response
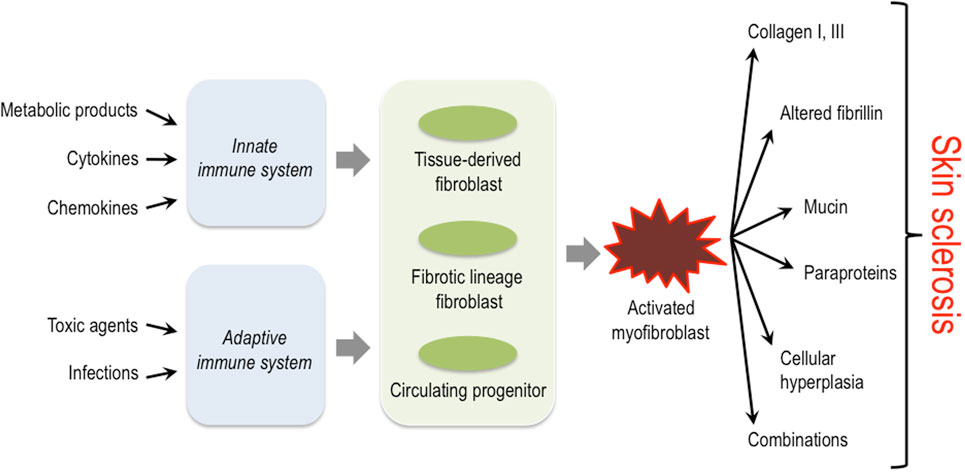
Scleroderma is classified as an autoimmune disease, meaning the immune system mistakenly attacks healthy tissues in the body. In this case, the immune system targets the cells responsible for producing collagen, leading to excessive collagen production and subsequent tissue damage.
Genetic Predisposition
While scleroderma is not directly inherited, certain genetic factors may increase an individual’s susceptibility to developing the condition. People with a family history of autoimmune diseases are at a higher risk.
Environmental Triggers
Exposure to certain environmental factors, such as silica dust, organic solvents, or viral infections, may trigger scleroderma in genetically predisposed individuals. However, more research is needed to fully understand these connections.
Hormonal Factors
Scleroderma is more common in women than men, suggesting that hormones may play a role in its development. Estrogen, in particular, has been studied for its potential influence on the immune system and collagen production.
Symptoms of Scleroderma
The symptoms of scleroderma vary depending on the type and severity of the condition. Some people experience mild symptoms, while others face life-threatening complications. Below are the most common signs and symptoms associated with scleroderma:
Skin Changes
- Thickened, tight, and shiny skin, particularly on the fingers, hands, and face.
- Patches of discolored skin, ranging from red to white, often seen in localized scleroderma.
- Ulcers or sores on the fingertips due to poor blood circulation.
Raynaud’s Phenomenon
One of the earliest and most common symptoms of scleroderma is Raynaud’s phenomenon, which causes the small blood vessels in the fingers and toes to constrict in response to cold or stress. This leads to color changes in the skin (white, blue, then red) and sensations of numbness, tingling, or pain.
Gastrointestinal Issues
- Difficulty swallowing due to esophageal dysfunction.
- Bloating, diarrhea, or constipation caused by slowed movement in the intestines.
- Acid reflux or heartburn resulting from weakened muscles in the esophagus.
Respiratory Problems
Scleroderma can affect the lungs, leading to conditions such as interstitial lung disease (scarring of lung tissue) or pulmonary arterial hypertension (high blood pressure in the arteries of the lungs). These complications can cause shortness of breath, persistent coughing, and fatigue.
Cardiovascular Symptoms
- High blood pressure, especially in cases where the kidneys are affected (renal crisis).
- Chest pain or irregular heartbeats due to inflammation of the heart muscle or surrounding tissues.
Musculoskeletal Symptoms
- Joint pain, stiffness, and swelling, similar to arthritis.
- Muscle weakness or cramps, particularly in the hands and feet.
Treatment Options for Scleroderma
There is currently no cure for scleroderma, but various treatments can help manage symptoms, slow disease progression, and improve quality of life. Treatment plans are tailored to each individual based on the type and severity of their condition.
Medications
- Immunosuppressants: Drugs like methotrexate or cyclophosphamide are used to suppress the overactive immune response in systemic scleroderma.
- Vasodilators: Medications such as calcium channel blockers or endothelin receptor antagonists help improve blood flow and reduce symptoms of Raynaud’s phenomenon.
- Anti-inflammatory Drugs: Nonsteroidal anti-inflammatory drugs (NSAIDs) can alleviate joint pain and inflammation.
- Antacids and Proton Pump Inhibitors: These medications address gastrointestinal issues like acid reflux and heartburn.
Physical and Occupational Therapy
Physical therapy can help maintain flexibility and strength in affected joints and muscles, while occupational therapy focuses on improving daily functioning and adapting to physical limitations. Stretching exercises, massage, and heat therapy are commonly recommended.
Management of Organ Complications
- Lung Involvement: Patients with interstitial lung disease may benefit from oxygen therapy or medications that reduce inflammation and scarring in the lungs.
- Kidney Issues: Angiotensin-converting enzyme inhibitors are often prescribed to control high blood pressure and prevent kidney damage during renal crises.
- Heart Problems: Cardiac medications, including beta-blockers or diuretics, may be used to manage heart-related symptoms.
Lifestyle Modifications
- Avoid exposure to cold temperatures to minimize Raynaud’s symptoms.
- Follow a balanced diet rich in fruits, vegetables, and fiber to support overall health and digestion.
- Quit smoking, as it worsens vascular problems and reduces blood flow.
- Engage in regular, low-impact exercise to improve circulation and maintain joint mobility.
Emerging Therapies
Research into scleroderma is ongoing, with promising advancements in stem cell transplantation and targeted therapies. Stem cell transplants aim to “reset” the immune system, while biologic drugs target specific pathways involved in the disease process. While these treatments are still being studied, they offer hope for better outcomes in the future.