Rheumatic Heart Disease, often abbreviated as RHD, is a serious condition that affects the heart valves and can lead to long-term complications if left untreated. This article explores the causes, symptoms, and care options for individuals dealing with this chronic illness. Understanding these aspects can help patients and caregivers manage the disease more effectively and improve quality of life.
Understanding Rheumatic Heart Disease
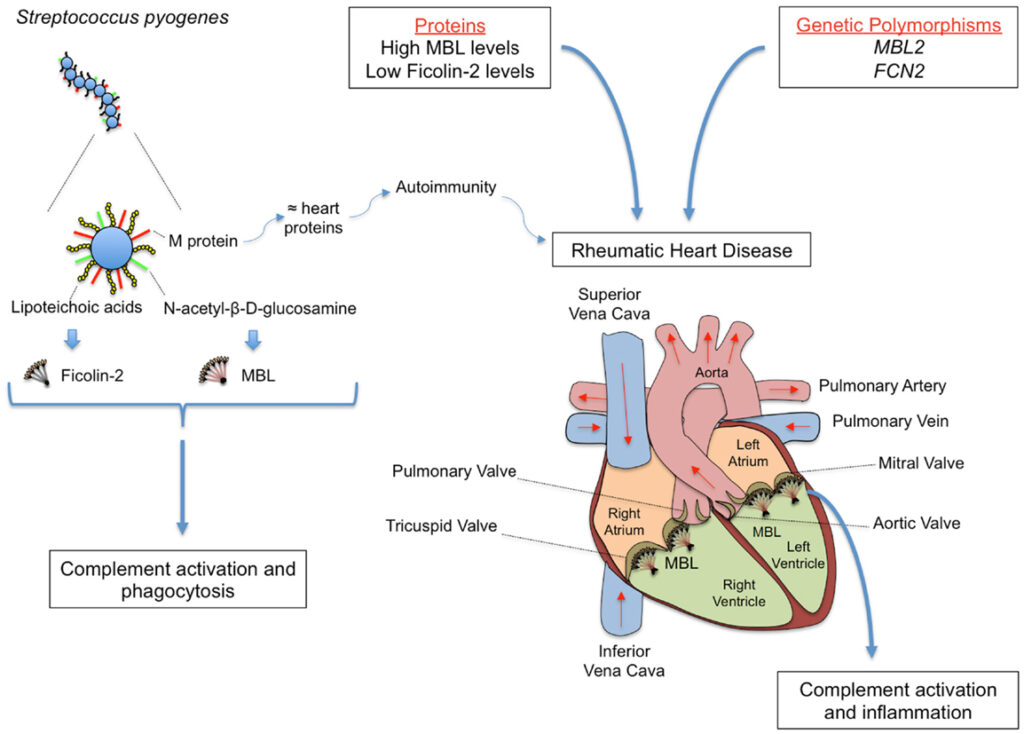
Rheumatic Heart Disease is a condition that arises as a complication of rheumatic fever, an inflammatory disease caused by an untreated or inadequately treated streptococcal infection. The disease primarily targets the heart valves, causing them to become inflamed, scarred, and dysfunctional over time. If not managed properly, it can result in heart failure, stroke, or even death.
The Role of Rheumatic Fever
Rheumatic fever is the precursor to Rheumatic Heart Disease. It occurs when a bacterial infection, typically strep throat or scarlet fever, is not treated promptly with antibiotics. The immune system’s response to the infection mistakenly attacks healthy tissues, particularly those in the heart, joints, skin, and brain. Over time, repeated episodes of rheumatic fever can damage the heart valves, leading to the development of Rheumatic Heart Disease.
Causes of Rheumatic Heart Disease
The primary cause of Rheumatic Heart Disease is an untreated or poorly treated streptococcal infection. However, several factors contribute to its development and progression:
Untreated Strep Throat or Scarlet Fever
- When strep throat or scarlet fever is left untreated, the bacteria responsible for the infection can trigger an abnormal immune response. This response may lead to inflammation of the heart tissues, eventually affecting the heart valves.
Repeated Episodes of Rheumatic Fever
- Individuals who experience multiple episodes of rheumatic fever are at a higher risk of developing Rheumatic Heart Disease. Each episode increases the likelihood of permanent damage to the heart valves.
Socioeconomic Factors
- Poverty, lack of access to healthcare, and overcrowded living conditions are significant contributors to the spread of streptococcal infections and the subsequent development of Rheumatic Heart Disease. These factors often prevent timely diagnosis and treatment of strep throat or scarlet fever.
Genetic Predisposition
- Some individuals may have a genetic predisposition that makes them more susceptible to developing Rheumatic Heart Disease after an episode of rheumatic fever. Research is ongoing to better understand the role of genetics in this condition.
Symptoms of Rheumatic Heart Disease
The symptoms of Rheumatic Heart Disease vary depending on the severity of the condition and which heart valves are affected. In some cases, symptoms may not appear until years after the initial episode of rheumatic fever. Common signs include:
Shortness of Breath
- One of the earliest and most noticeable symptoms is shortness of breath, especially during physical activity or while lying down. This occurs because the damaged heart valves make it harder for the heart to pump blood efficiently.
Fatigue
- Patients often experience persistent fatigue, even after minimal exertion. This is due to the heart’s reduced ability to supply oxygen-rich blood to the body.
Chest Pain
- Chest pain or discomfort may occur, particularly during physical activity. This symptom is a result of the heart working harder to compensate for the damaged valves.
Swelling
- Swelling in the ankles, feet, or abdomen is a common sign of fluid retention, which happens when the heart cannot pump blood effectively. This can also lead to weight gain.
Heart Palpitations
- Irregular or rapid heartbeats, known as palpitations, may occur as the heart struggles to maintain normal function. These palpitations can sometimes be felt as fluttering sensations in the chest.
Fainting or Dizziness
- In severe cases, individuals may experience fainting spells or dizziness due to inadequate blood flow to the brain.
Diagnosis of Rheumatic Heart Disease
Early diagnosis is crucial for managing Rheumatic Heart Disease effectively. Healthcare providers use a combination of methods to identify the condition:
Medical History and Physical Examination
- A detailed medical history, including any past episodes of rheumatic fever, is essential for diagnosis. During a physical examination, doctors listen for abnormal heart sounds, such as murmurs, which may indicate valve damage.
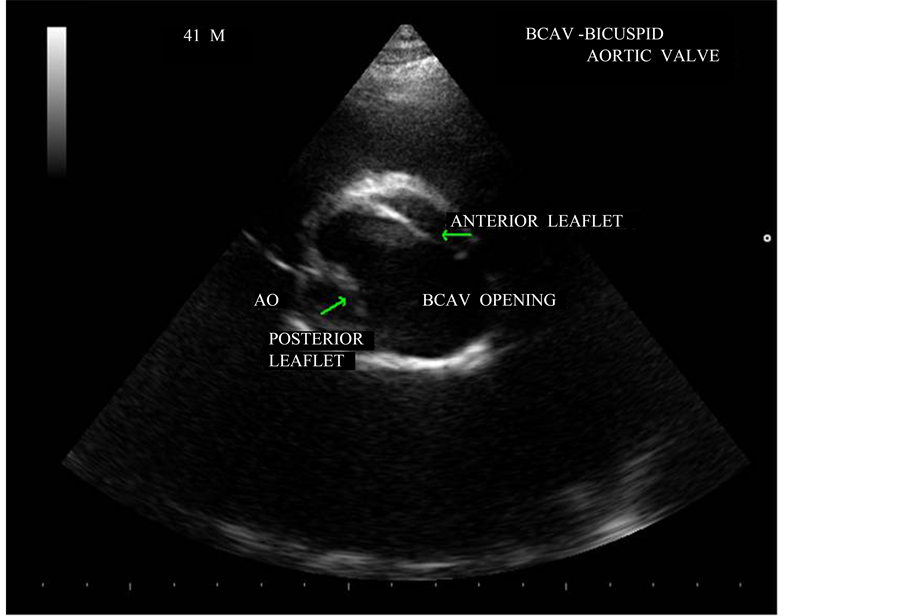
Echocardiogram
- An echocardiogram is a non-invasive imaging test that uses sound waves to create detailed pictures of the heart. This test helps doctors assess the structure and function of the heart valves and identify any abnormalities.
Electrocardiogram (ECG)
- An electrocardiogram measures the electrical activity of the heart and can detect irregular heart rhythms or signs of heart enlargement, both of which may be associated with Rheumatic Heart Disease.
Blood Tests
- Blood tests may be performed to check for markers of inflammation or infection, which can provide additional clues about the presence of rheumatic fever or its complications.
Treatment and Care Options
While there is no cure for Rheumatic Heart Disease, various treatments and care strategies can help manage symptoms and prevent further damage to the heart. The approach depends on the severity of the condition and the specific needs of the patient.
Antibiotics
- Long-term antibiotic therapy is often prescribed to prevent recurrent episodes of rheumatic fever, which can worsen heart valve damage. Patients may need to take antibiotics regularly for many years, sometimes even for life.
Medications to Manage Symptoms
- Doctors may prescribe medications such as diuretics to reduce fluid buildup, beta-blockers to control heart rate, and anticoagulants to prevent blood clots. These medications help alleviate symptoms and improve overall heart function.
Surgical Interventions
- In severe cases, surgery may be necessary to repair or replace damaged heart valves. Valve repair involves fixing the existing valve, while valve replacement involves substituting the damaged valve with a mechanical or biological one.
Lifestyle Modifications
- Making certain lifestyle changes can significantly improve the quality of life for individuals with Rheumatic Heart Disease. These include adopting a heart-healthy diet, engaging in regular low-impact exercise, quitting smoking, and managing stress.
Regular Monitoring and Follow-Up
- Regular check-ups with a cardiologist are essential for monitoring the progression of the disease and adjusting treatment plans as needed. Early detection of complications can prevent further damage and improve outcomes.
Preventing Rheumatic Heart Disease
Prevention is key to reducing the incidence of Rheumatic Heart Disease. By addressing the root causes and implementing preventive measures, the risk of developing this condition can be minimized.
Timely Treatment of Strep Throat
- Seeking prompt medical attention for strep throat or scarlet fever is critical. A course of antibiotics can effectively treat the infection and prevent the onset of rheumatic fever.
Vaccination and Public Health Initiatives
- Public health programs aimed at improving access to healthcare, promoting hygiene, and raising awareness about the importance of treating streptococcal infections can significantly reduce the burden of Rheumatic Heart Disease, especially in low-income communities.
Education and Awareness
- Educating communities about the signs and symptoms of strep throat, rheumatic fever, and Rheumatic Heart Disease can empower individuals to seek timely medical care and adhere to treatment plans.
Living with Rheumatic Heart Disease
Managing Rheumatic Heart Disease requires a comprehensive approach that includes medical treatment, lifestyle adjustments, and emotional support. Patients and their families should work closely with healthcare providers to develop a personalized care plan that addresses their unique needs.
Emotional and Psychological Support
- Living with a chronic illness can be emotionally challenging. Counseling, support groups, and open communication with loved ones can help individuals cope with the psychological impact of Rheumatic Heart Disease.
Empowering Patients Through Education
- Understanding the disease and its management empowers patients to take an active role in their care. Learning about medication schedules, recognizing warning signs, and knowing when to seek medical help are all important aspects of self-care.