Retinal detachment, often abbreviated as RD, is a serious eye condition that requires immediate medical attention. It occurs when the retina, a thin layer of tissue at the back of the eye responsible for capturing light and sending signals to the brain, pulls away from its normal position. If left untreated, this condition can lead to permanent vision loss. Understanding the causes, recognizing the symptoms, and knowing how to diagnose and treat retinal detachment are essential for preserving eyesight.

What Is Retinal Detachment?
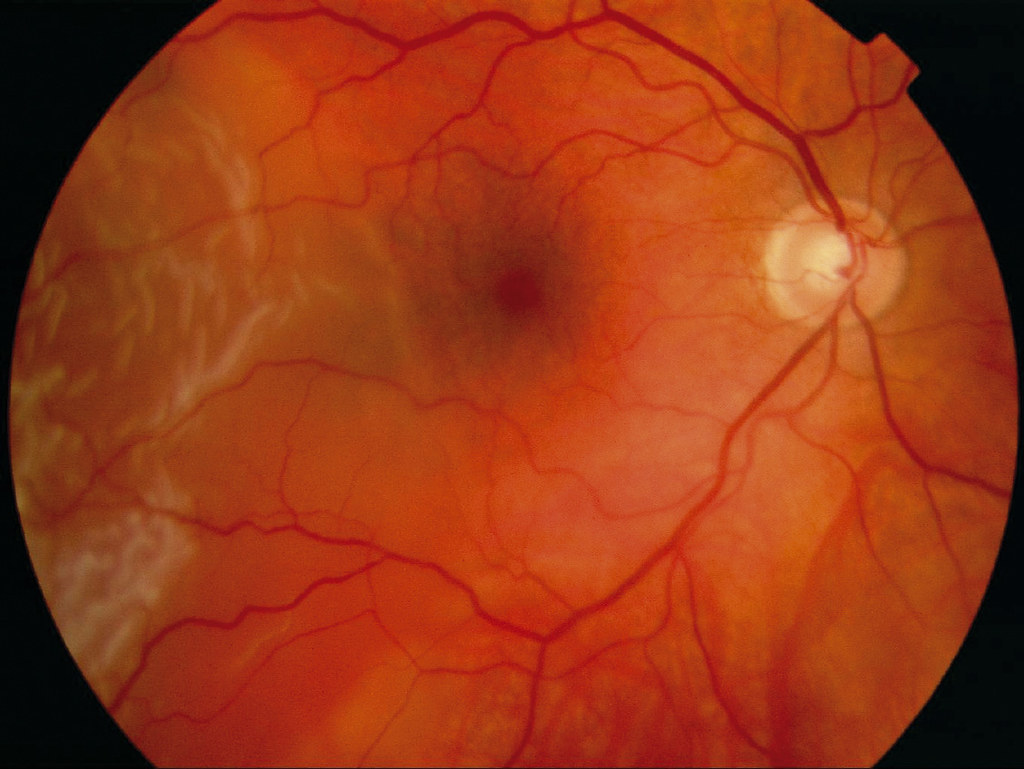
The retina is a vital part of the eye that plays a crucial role in vision. It contains millions of light-sensitive cells that detect images and send them to the brain through the optic nerve. When the retina detaches, it loses its blood supply and ability to function properly. This separation disrupts the flow of visual information, leading to blurred vision or even blindness if not addressed promptly.
There are three main types of retinal detachment:
- Rhegmatogenous: This is the most common type and occurs when a tear or hole in the retina allows fluid to pass underneath, causing the retina to detach.
- Tractional: This type happens when scar tissue on the retina’s surface contracts and pulls the retina away from its underlying support.
- Exudative: In this form, fluid accumulates beneath the retina without any tears or breaks, often due to inflammation, injury, or other underlying conditions.
Causes of Retinal Detachment
Several factors can increase the risk of retinal detachment. While some causes are related to age and natural changes in the eye, others may result from trauma or pre-existing health conditions. Below are the primary causes:
Age-Related Changes
As people grow older, the vitreous, a gel-like substance that fills the center of the eye, begins to shrink and pull away from the retina. This process, known as posterior vitreous detachment, is a normal part of aging but can sometimes cause tears in the retina. These tears can progress to full detachment if not treated early.
Injury or Trauma
Severe injuries to the eye or head can damage the retina and lead to detachment. Sports-related accidents, car crashes, or blunt force trauma are common examples. Even minor injuries should be evaluated by an eye care professional to rule out potential complications.
Previous Eye Surgeries
Individuals who have undergone eye surgeries, such as cataract removal, are at a higher risk of developing retinal detachment. The surgical procedure can alter the structure of the eye, making it more susceptible to tears or detachment.
Family History and Genetic Factors
A family history of retinal detachment increases the likelihood of experiencing the condition. Some inherited disorders, such as Stickler syndrome or Marfan syndrome, also predispose individuals to retinal problems.
Other Medical Conditions
Certain systemic diseases, such as diabetes, can affect the health of the retina. Diabetic retinopathy, for instance, weakens the blood vessels in the retina and may contribute to tractional retinal detachment. Additionally, inflammatory conditions like uveitis can lead to exudative retinal detachment.
Symptoms of Retinal Detachment
Recognizing the symptoms of retinal detachment is critical for seeking timely treatment. Unlike some medical conditions, retinal detachment does not cause pain, so individuals must pay close attention to visual changes. Common symptoms include:
Sudden Appearance of Floaters
Floaters are small specks or cobweb-like shapes that drift across your field of vision. While occasional floaters are normal, a sudden increase in their number can indicate a problem with the retina.
Flashes of Light
Brief flashes of light, especially in peripheral vision, may occur when the retina is stimulated by tugging or pulling forces. These flashes often resemble lightning streaks and can appear intermittently.
Shadow or Curtain Over Vision
One of the hallmark signs of retinal detachment is the sensation of a shadow or curtain descending over part of your vision. This symptom typically starts at the edges and progresses toward the center.
Blurred or Distorted Vision
Vision may become blurry or distorted as the retina loses its connection to the underlying tissue. Straight lines may appear wavy, and objects may seem out of focus.
Loss of Peripheral Vision
Peripheral vision, also known as side vision, may diminish as the retina detaches. This reduction can make it difficult to see objects outside the central field of view.
Diagnosis of Retinal Detachment
If you experience any of the above symptoms, it is important to consult an eye care specialist immediately. A comprehensive eye examination is necessary to confirm the presence of retinal detachment. During the diagnostic process, the following steps are typically involved:
Dilated Eye Exam
An ophthalmologist will use special eye drops to dilate the pupils, allowing for a clearer view of the retina. Using a bright light and magnifying lens, they will inspect the back of the eye for signs of tears, holes, or detachment.
Ultrasound Imaging
In cases where bleeding or cloudiness prevents a clear view of the retina, ultrasound imaging may be used. This non-invasive technique uses sound waves to create detailed pictures of the eye’s internal structures.
Optical Coherence Tomography
This advanced imaging method provides cross-sectional images of the retina, helping doctors assess its thickness and identify areas of detachment or swelling.
Treatment Options for Retinal Detachment
Timely intervention is crucial to prevent permanent vision loss. The treatment approach depends on the type, severity, and location of the detachment. Here are the most common methods used to repair a detached retina:
Laser Surgery
Laser surgery, also known as photocoagulation, is often used to seal small retinal tears before they progress to detachment. During the procedure, a laser beam creates tiny burns around the tear, forming scar tissue that holds the retina in place.
Cryopexy
Cryopexy involves freezing the area around the retinal tear using a probe. The freezing process induces scar tissue formation, which helps reattach the retina to the underlying tissue.
Pneumatic Retinopexy
This minimally invasive procedure is suitable for certain types of retinal detachment. A gas bubble is injected into the vitreous cavity, where it presses against the detached retina and pushes it back into position. Laser or cryopexy is then performed to seal the tear.
Scleral Buckling
Scleral buckling is a surgical technique that involves placing a silicone band around the outside of the eye. The band gently indents the wall of the eye, reducing tension on the retina and allowing it to settle back into place.
Vitrectomy
In more complex cases, a vitrectomy may be required. During this procedure, the vitreous gel is removed from the eye and replaced with a saline solution or gas bubble. This allows the surgeon to access and repair the retina directly.
Recovery and Follow-Up Care
After undergoing treatment for retinal detachment, patients must adhere to specific recovery guidelines to ensure optimal healing. Depending on the procedure, recovery times can vary from a few weeks to several months. Key aspects of post-treatment care include:
Positioning Requirements
For procedures involving gas bubbles, patients may need to maintain a specific head position for extended periods. This positioning helps keep the bubble in contact with the detached area until the retina heals.
Activity Restrictions
Strenuous activities, heavy lifting, and bending over should be avoided during the initial recovery phase. These actions can increase pressure within the eye and interfere with healing.
Regular Check-Ups
Frequent follow-up appointments are essential to monitor the retina’s progress and address any complications. Your doctor may perform additional tests to ensure the retina remains securely attached.
Preventing Retinal Detachment
While not all cases of retinal detachment can be prevented, certain measures can reduce the risk:
- Regular eye exams, especially for individuals over the age of fifty or those with a family history of retinal issues.
- Wearing protective eyewear during sports or activities that pose a risk of eye injury.
- Managing underlying health conditions, such as diabetes, to minimize their impact on eye health.
- Seeking prompt medical attention for any sudden changes in vision.