A rectocele, also known as posterior vaginal wall prolapse, is a medical condition that affects many women, particularly after childbirth or during menopause. While it may not be widely discussed, understanding this condition is essential for those who experience its symptoms or are at risk of developing it. In this article, we will explore what a rectocele is, its causes, common symptoms, diagnostic methods, and available treatments to help individuals make informed decisions about their health.

What Is a Rectocele?
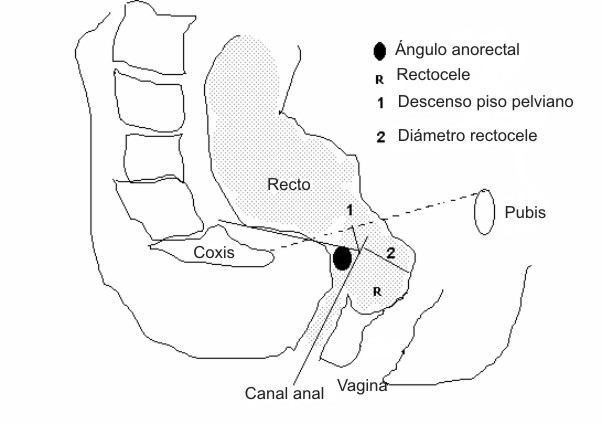
A rectocele occurs when the thin wall of tissue separating the rectum from the vagina weakens or stretches, causing the rectum to bulge into the back wall of the vagina. This can lead to discomfort, difficulty with bowel movements, and other related issues. The severity of the condition can vary, ranging from mild cases that cause no noticeable symptoms to more severe instances that significantly impact daily life.
The weakening of the pelvic floor muscles and connective tissues often plays a significant role in the development of a rectocele. These structures support the pelvic organs, including the bladder, uterus, and rectum. When they become compromised, the risk of prolapse increases.
Common Causes of a Rectocele
Several factors can contribute to the development of a rectocele. Some of the most common causes include:
- Childbirth: Vaginal delivery, especially if it involves prolonged labor or the use of forceps, can stretch and damage the pelvic floor muscles and tissues.
- Aging: As women age, particularly after menopause, the levels of estrogen decrease. This hormone helps maintain the strength and elasticity of pelvic tissues, so its decline can increase the risk of prolapse.
- Chronic Straining: Regular straining during bowel movements due to constipation or chronic coughing can place excessive pressure on the pelvic floor, leading to weakening over time.
- Obesity: Excess body weight can put additional strain on the pelvic floor, increasing the likelihood of developing a rectocele.
- Prior Pelvic Surgery: Surgeries involving the pelvic region, such as hysterectomy, may alter the structural integrity of the pelvic floor and contribute to prolapse.
Symptoms of a Rectocele
The symptoms of a rectocele can vary depending on its severity. Some women may experience no symptoms at all, while others may notice significant discomfort or functional difficulties. Common signs and symptoms include:
- A Bulge or Lump: Many women report feeling a noticeable bulge in the vagina, which may become more prominent when standing or straining.
- Difficulty with Bowel Movements: A rectocele can create a pocket where stool becomes trapped, making it difficult to fully empty the bowels. This often leads to the need to press on the back wall of the vagina to facilitate bowel movements.
- Pelvic Pressure or Discomfort: Women with a rectocele may feel a sense of fullness, pressure, or heaviness in the pelvic area, particularly after standing for long periods or at the end of the day.
- Urinary or Fecal Incontinence: In some cases, a rectocele can affect bladder or bowel control, leading to leakage of urine or stool.
- Pain During Sexual Intercourse: The presence of a rectocele may cause discomfort or pain during sexual activity.
It is important to note that these symptoms can overlap with other pelvic floor disorders, such as cystocele (bladder prolapse) or uterine prolapse. Therefore, a thorough evaluation by a healthcare professional is necessary for an accurate diagnosis.
Diagnosing a Rectocele
To diagnose a rectocele, a healthcare provider will typically begin with a detailed medical history and physical examination. During the pelvic exam, the doctor may ask the patient to bear down or strain as if having a bowel movement. This maneuver helps reveal any bulging or prolapse of the rectum into the vagina.
In some cases, additional tests may be recommended to assess the severity of the condition and rule out other potential causes of symptoms. These tests may include:
- Imaging Studies: Ultrasound or magnetic resonance imaging may provide detailed images of the pelvic organs to evaluate the extent of the prolapse.
- Defecography: This specialized X-ray procedure involves filling the rectum with a contrast material to observe how the rectum and surrounding structures function during a bowel movement.
- Anorectal Manometry: This test measures the strength and coordination of the muscles involved in bowel movements.
Treatment Options for a Rectocele
The treatment approach for a rectocele depends on the severity of symptoms, the impact on quality of life, and the patient’s overall health. In mild cases, conservative measures may be sufficient to manage symptoms. For more severe cases, surgical intervention may be necessary.
Non-Surgical Treatments
For women with mild to moderate symptoms, non-surgical treatments are often the first line of management. These options aim to strengthen the pelvic floor muscles and alleviate discomfort. Common non-surgical approaches include:
- Pelvic Floor Exercises: Also known as Kegel exercises, these involve contracting and relaxing the pelvic floor muscles to improve their strength and endurance. A physical therapist specializing in pelvic health can provide guidance on proper technique.
- Dietary Changes: Increasing fiber intake and staying hydrated can help prevent constipation, reducing the need for straining during bowel movements.
- Vaginal Pessaries: These are removable devices inserted into the vagina to support the prolapsed tissue. They can provide temporary relief from symptoms and are often used by women who wish to avoid surgery or are not good candidates for it.
- Hormone Therapy: For postmenopausal women, topical estrogen therapy may help restore the health of vaginal tissues and improve symptoms.
Surgical Treatments
If non-surgical treatments fail to provide adequate relief or if the rectocele is severe, surgery may be considered. The goal of surgery is to repair the weakened tissues and restore normal anatomy. There are several surgical techniques available, and the choice depends on the individual’s specific needs and preferences. Common procedures include:
- Posterior Colporrhaphy: This traditional surgical approach involves folding and suturing the stretched tissues of the vaginal wall to reinforce the area and correct the prolapse.
- Mesh Augmentation: In some cases, synthetic mesh may be used to provide additional support to the repaired tissues. However, the use of mesh is controversial due to potential complications, such as infection or erosion.
- Laparoscopic or Robotic Surgery: Minimally invasive techniques, such as laparoscopy or robotic-assisted surgery, allow for smaller incisions, reduced recovery time, and less postoperative pain compared to traditional open surgery.
Before undergoing surgery, patients should discuss the risks, benefits, and expected outcomes with their healthcare provider to ensure they are making an informed decision.
Preventing a Rectocele
While not all cases of rectocele can be prevented, certain lifestyle modifications can reduce the risk of developing this condition or prevent it from worsening. These preventive measures include:
- Maintaining a Healthy Weight: Excess weight places additional strain on the pelvic floor, so maintaining a healthy body mass index can help protect against prolapse.
- Avoiding Chronic Straining: Addressing underlying conditions that cause chronic straining, such as constipation or chronic cough, can help preserve pelvic floor integrity.
- Strengthening the Pelvic Floor: Regular pelvic floor exercises can enhance muscle tone and support the pelvic organs.
- Practicing Safe Lifting Techniques: Lifting heavy objects improperly can put undue pressure on the pelvic floor, so using proper techniques is essential.
Women who have experienced childbirth or are approaching menopause should pay particular attention to these preventive strategies, as they are at higher risk for developing pelvic floor disorders.
When to Seek Medical Attention
Women who experience persistent symptoms of a rectocele or notice a significant impact on their quality of life should consult a healthcare provider. Early intervention can help prevent the condition from worsening and improve overall outcomes. Additionally, individuals who develop new or worsening symptoms after treatment should seek medical advice promptly.
It is also important to address any coexisting pelvic floor disorders, as these conditions often occur together and may require a comprehensive treatment plan.