Rectal prolapse, also known as RP, is a medical condition where the rectum, which is the lower part of the large intestine, protrudes out of the anus. This can occur partially or completely, causing discomfort and other complications. While it is not life-threatening, rectal prolapse can significantly impact a person’s quality of life if left untreated. Understanding its causes, symptoms, diagnosis, and treatment options is essential for managing this condition effectively.
What Is Rectal Prolapse?
Rectal prolapse happens when the rectal walls lose their attachment to surrounding tissues and muscles, causing them to slip downward. In some cases, only the lining of the rectum protrudes, while in more severe instances, the entire rectal wall may come out. This condition is more common in older adults, particularly women, but it can affect people of all ages, including children.
Causes of Rectal Prolapse
The exact cause of rectal prolapse is often multifactorial, meaning several factors contribute to its development. Below are some of the most common causes:
Weak Pelvic Floor Muscles
Pelvic floor muscles play a crucial role in supporting the rectum and other pelvic organs. When these muscles weaken due to aging, childbirth, or chronic straining, the rectum may lose its support and begin to slip out of place.
Chronic Constipation
Frequent straining during bowel movements can put excessive pressure on the rectum and pelvic floor. Over time, this can lead to weakening of the supportive tissues and result in rectal prolapse.
Pregnancy and Childbirth
Pregnancy and vaginal childbirth can stretch and damage the pelvic muscles and ligaments. Women who have had multiple pregnancies or difficult deliveries are at a higher risk of developing this condition.
Aging
As people age, the muscles and connective tissues in the body naturally weaken. This makes older adults more susceptible to rectal prolapse, especially those over the age of 50.
Previous Surgeries
Certain surgeries involving the pelvic area, such as hysterectomies or prostate surgeries, can alter the anatomy and weaken the structures that hold the rectum in place.
Neurological Disorders
Conditions like multiple sclerosis, spinal cord injuries, or long-standing diabetes can interfere with nerve signals to the pelvic muscles. This can lead to poor muscle coordination and increase the likelihood of rectal prolapse.
Symptoms of Rectal Prolapse
The symptoms of rectal prolapse can vary depending on the severity of the condition. Some individuals may experience mild discomfort, while others may face significant challenges. Common symptoms include:
- Visible Bulge: A noticeable lump or bulge protruding from the anus, especially during bowel movements or physical activity.
- Pain or Discomfort: Individuals may feel pain or discomfort in the rectal area, particularly when sitting or walking.
- Bleeding: The protruding rectal tissue may become irritated or bleed, leading to blood in the stool or on toilet paper.
- Mucus Discharge: Increased mucus production can occur, resulting in leakage or soiling of undergarments.
- Incontinence: Some people may experience difficulty controlling bowel movements or gas due to weakened sphincter muscles.
- Sensation of Fullness: A feeling of fullness or incomplete evacuation even after using the bathroom.
Diagnosis of Rectal Prolapse
Diagnosing rectal prolapse typically involves a combination of physical examinations, medical history reviews, and diagnostic tests. Here’s how healthcare providers identify this condition:
Physical Examination
A doctor will perform a thorough physical examination to assess the extent of the prolapse. During this exam, they may ask the patient to bear down or simulate a bowel movement to observe the protrusion.
Medical History Review
Understanding the patient’s medical history is vital. Doctors will inquire about symptoms, lifestyle habits, previous surgeries, and any underlying health conditions that could contribute to the prolapse.
Imaging Tests
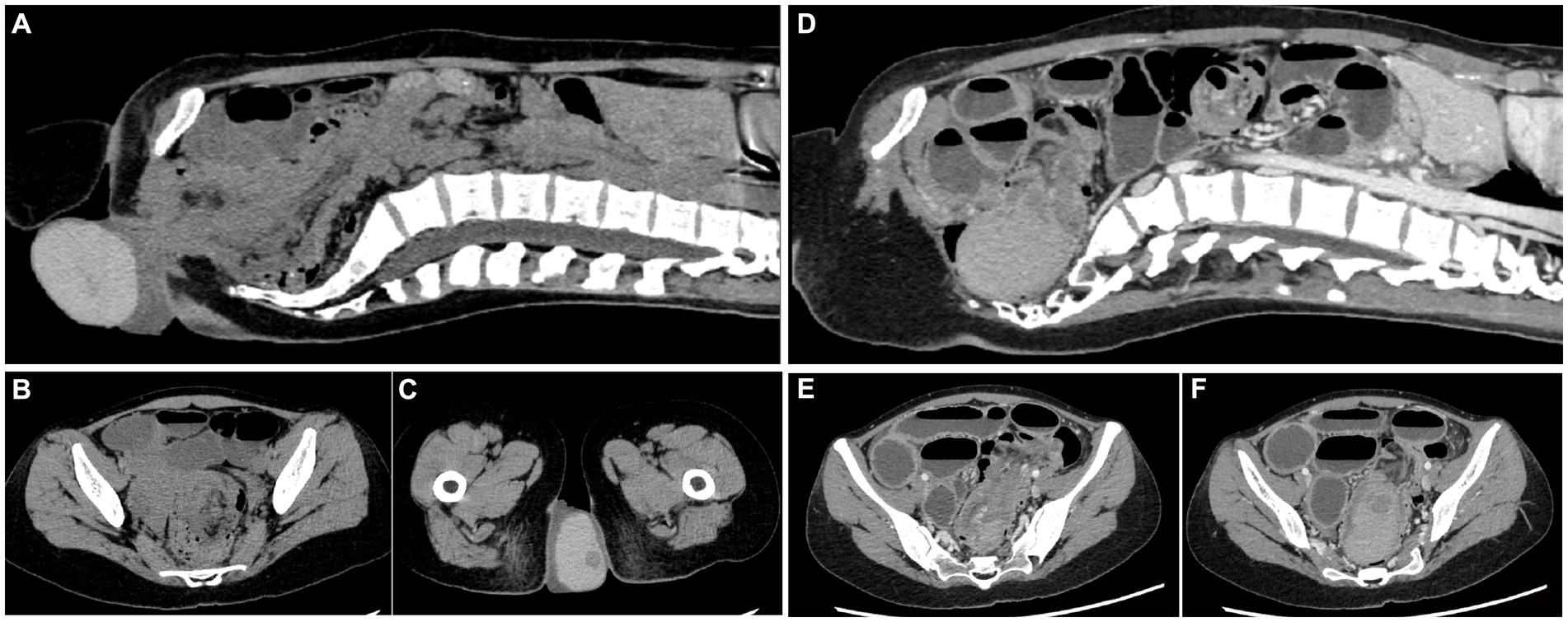
In some cases, imaging tests such as an ultrasound, MRI, or defecography may be used to evaluate the structure and function of the pelvic floor and rectum. These tests help determine the severity of the prolapse and guide treatment decisions.
Colonoscopy
A colonoscopy may be recommended to rule out other potential causes of symptoms, such as tumors or inflammatory bowel disease. This procedure allows doctors to examine the entire colon and rectum closely.
Treatment Options for Rectal Prolapse
Treatment for rectal prolapse depends on the severity of the condition, the patient’s overall health, and their preferences. Both non-surgical and surgical approaches are available, each with its own benefits and risks.
Non-Surgical Treatments
For mild cases of rectal prolapse, non-surgical treatments may be sufficient to manage symptoms. These include:
- Dietary Changes: Increasing fiber intake through fruits, vegetables, and whole grains can soften stools and reduce straining during bowel movements.
- Hydration: Drinking plenty of water helps maintain regular bowel movements and prevents constipation.
- Pelvic Floor Exercises: Strengthening exercises, such as Kegels, can improve muscle tone and provide better support for the rectum.
- Laxatives: In some cases, over-the-counter or prescription laxatives may be prescribed to relieve constipation and minimize straining.
Surgical Treatments
If non-surgical methods fail or if the prolapse is severe, surgery may be necessary. There are two main types of surgical procedures for rectal prolapse:
Abdominal Surgery
This approach involves making incisions in the abdomen to reposition the rectum and secure it in place. Abdominal surgery is typically recommended for younger, healthier patients and offers a lower risk of recurrence compared to other methods.
Perineal Surgery
Perineal surgery is performed through the area between the anus and genitals. It is less invasive than abdominal surgery and is often preferred for older adults or those with significant health issues. However, it carries a slightly higher risk of recurrence.
Post-Surgery Recovery
After surgery, patients are advised to follow specific recovery guidelines to ensure proper healing. These may include:
- Avoiding heavy lifting and strenuous activities for several weeks.
- Following a high-fiber diet to prevent constipation.
- Taking prescribed medications to manage pain and prevent infections.
- Attending follow-up appointments to monitor progress and address any concerns.
Preventing Rectal Prolapse
While not all cases of rectal prolapse can be prevented, certain measures can reduce the risk of developing this condition:
- Maintain a healthy weight to avoid putting extra pressure on the pelvic floor.
- Practice good bowel habits by avoiding prolonged sitting on the toilet and refraining from straining during bowel movements.
- Engage in regular exercise to strengthen core and pelvic muscles.
- Seek prompt treatment for chronic constipation or diarrhea to minimize strain on the rectum.