Rectal cancer, often grouped under the broader term colorectal cancer (CRC), is a significant health concern worldwide. It originates in the rectum, the final section of the large intestine that connects to the anus. Understanding its causes, recognizing its symptoms, and being aware of diagnostic methods and treatment options are crucial for early detection and effective management. This article delves into the details of rectal cancer, providing comprehensive insights into its various aspects.

Understanding Rectal Cancer
Rectal cancer occurs when abnormal cells grow uncontrollably in the lining of the rectum. Over time, these cells can invade nearby tissues and spread to other parts of the body, leading to severe complications if left untreated. While it shares similarities with colon cancer, rectal cancer has distinct characteristics due to its location and the challenges associated with treating tumors near the anus.
Risk Factors and Causes
Several factors contribute to the development of rectal cancer. Some of these are lifestyle-related, while others are beyond an individual’s control. Below is a detailed breakdown:
- Age: The risk of developing rectal cancer increases with age, particularly after the age of fifty.
- Family History: Individuals with a family history of rectal or colon cancer are at a higher risk. Certain inherited conditions, such as familial adenomatous polyposis and Lynch syndrome, also elevate the likelihood of developing this disease.
- Diet: A diet high in red meat, processed foods, and low in fiber may increase the risk of rectal cancer. Conversely, diets rich in fruits, vegetables, and whole grains are associated with a lower risk.
- Inflammatory Bowel Disease: Chronic inflammatory conditions like ulcerative colitis and Crohn’s disease can significantly raise the chances of developing rectal cancer.
- Sedentary Lifestyle: Lack of physical activity has been linked to an increased risk of rectal cancer.
- Obesity: Being overweight or obese is another contributing factor.
- Smoking and Alcohol Consumption: Both smoking and excessive alcohol intake have been identified as risk factors.
Recognizing the Symptoms
Identifying the symptoms of rectal cancer early can make a significant difference in treatment outcomes. However, it is important to note that early-stage rectal cancer may not present noticeable symptoms. As the disease progresses, the following signs may become apparent:
- Blood in Stool: One of the most common symptoms is the presence of blood in the stool, which may appear bright red or dark.
- Changes in Bowel Habits: Persistent diarrhea, constipation, or changes in stool consistency can indicate underlying issues.
- Abdominal Discomfort: Cramps, pain, or bloating in the abdominal area may occur.
- Unexplained Weight Loss: Sudden and unintended weight loss is often a red flag for various cancers, including rectal cancer.
- Fatigue: Persistent tiredness or weakness may result from chronic blood loss or the body’s response to cancer.
- Sensation of Incomplete Bowel Movement: Feeling as though the bowel does not empty completely after a bowel movement is another potential symptom.
Diagnosing Rectal Cancer
Early diagnosis is critical for improving survival rates and treatment success. Healthcare providers use a combination of methods to diagnose rectal cancer accurately. These include:
Physical Examination and Medical History
A healthcare provider will begin by conducting a thorough physical examination and reviewing the patient’s medical history. This helps identify any risk factors or symptoms that warrant further investigation.
Digital Rectal Exam
This simple procedure involves the doctor inserting a gloved, lubricated finger into the rectum to feel for abnormalities such as lumps or irregularities in the rectal wall.
Colonoscopy
A colonoscopy is a key diagnostic tool used to examine the entire length of the colon and rectum. During this procedure, a flexible tube with a camera is inserted through the anus to visualize the inner lining of the rectum and colon. If suspicious areas are found, biopsies can be taken for further analysis.
Imaging Tests
Imaging tests play a vital role in determining the extent of the cancer and whether it has spread to other parts of the body. Common imaging techniques include:
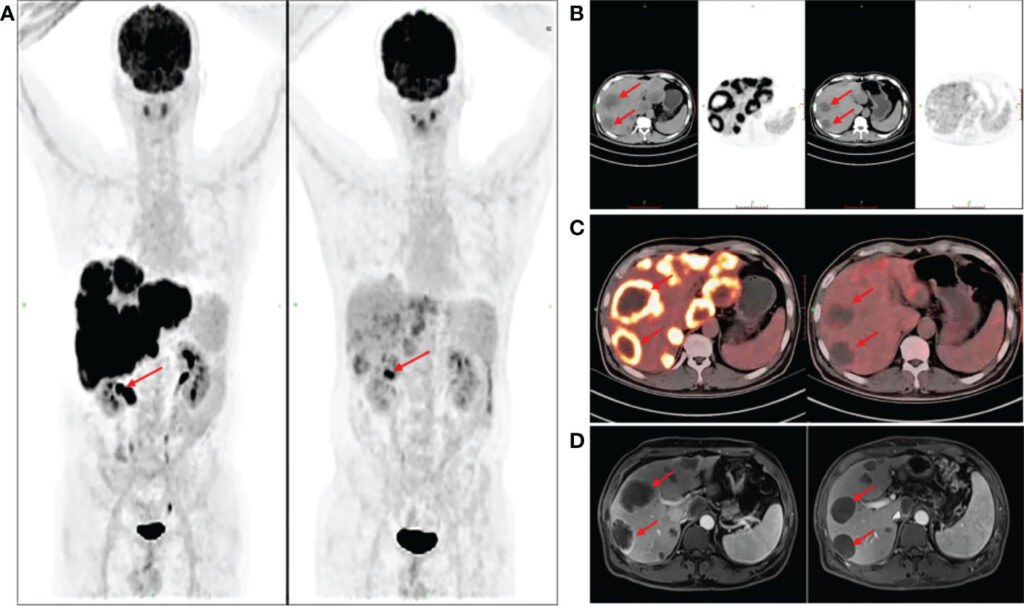
- Magnetic Resonance Imaging: MRI scans provide detailed images of the rectum and surrounding tissues, helping doctors assess the size and location of tumors.
- Computed Tomography Scan: CT scans create cross-sectional images of the body, aiding in staging the cancer and identifying metastasis.
- Pet Scan: Positron emission tomography scans help detect cancerous cells throughout the body by highlighting areas of high metabolic activity.
Laboratory Tests
Blood tests, including a complete blood count, may reveal anemia caused by chronic blood loss. Additionally, tumor markers like carcinoembryonic antigen levels can sometimes be elevated in individuals with rectal cancer.
Treatment Options for Rectal Cancer
The treatment plan for rectal cancer depends on several factors, including the stage of the cancer, the patient’s overall health, and personal preferences. Treatment approaches typically involve a combination of surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy.
Surgery
Surgical intervention is often the primary treatment for rectal cancer. The type of surgery performed depends on the size, location, and stage of the tumor:
- Local Excision: For small, early-stage tumors, surgeons may remove the cancerous tissue along with a margin of healthy tissue without cutting into the abdomen.
- Total Mesorectal Excision: This procedure involves removing the rectum and surrounding fatty tissue containing lymph nodes. It is commonly used for more advanced cancers.
- Colostomy or Ileostomy: In some cases, a stoma (an opening on the abdomen) may be created to allow waste to exit the body into a bag. This may be temporary or permanent depending on the extent of the surgery.
Radiation Therapy
Radiation therapy uses high-energy beams to kill cancer cells. It is often used before surgery to shrink tumors or after surgery to destroy remaining cancer cells. Radiation can also be employed as a palliative measure to relieve symptoms in advanced stages.
Chemotherapy
Chemotherapy involves the use of drugs to destroy cancer cells. It is frequently combined with radiation therapy (chemoradiation) before or after surgery. Chemotherapy may also be administered to treat metastatic rectal cancer that has spread to other organs.
Targeted Therapy
Targeted therapies focus on specific molecules involved in cancer growth and progression. These treatments are designed to block the action of these molecules, thereby inhibiting the spread of cancer. Targeted therapy is usually reserved for advanced cases where standard treatments have proven ineffective.
Immunotherapy
Immunotherapy harnesses the power of the immune system to fight cancer. Certain medications can enhance the body’s natural defenses to recognize and attack cancer cells. While still under research for rectal cancer, immunotherapy shows promise in treating specific subtypes of the disease.
Living with Rectal Cancer
Managing rectal cancer extends beyond medical treatments. Emotional and psychological support, dietary adjustments, and lifestyle modifications are essential components of care. Support groups, counseling, and educational resources can empower patients and their families to navigate the challenges posed by the disease.
Additionally, maintaining open communication with healthcare providers ensures that patients receive personalized care tailored to their unique needs. Regular follow-ups and adherence to treatment plans are crucial for monitoring progress and addressing any complications promptly.