Reactive arthritis, often abbreviated as ReA, is a type of inflammatory arthritis that develops in response to an infection elsewhere in the body. It typically affects the joints, but it can also impact other parts of the body, including the eyes, skin, and urinary tract. This condition is part of a group of disorders known as spondyloarthropathies, which share similar characteristics such as inflammation of the spine and large joints. In this article, we will explore the causes, symptoms, diagnosis, and treatment options for reactive arthritis.
What Causes Reactive Arthritis?
Reactive arthritis occurs when the immune system overreacts to an infection. The infection itself does not directly affect the joints, but it triggers an abnormal immune response that leads to inflammation in various parts of the body. While the exact cause of this immune reaction is not fully understood, certain infections are commonly associated with the development of reactive arthritis.
Infections That Trigger Reactive Arthritis
- Gastrointestinal Infections: Bacterial infections in the digestive tract, such as those caused by Salmonella, Shigella, Campylobacter, and Yersinia, are common triggers. These infections often result from consuming contaminated food or water.
- Sexually Transmitted Infections: Chlamydia trachomatis, a bacterium responsible for sexually transmitted infections, is another frequent cause. Reactive arthritis triggered by chlamydia is more common in young adults and tends to affect men more than women.
Risk Factors
While anyone can develop reactive arthritis, certain factors increase the likelihood of its occurrence:
- A genetic predisposition, particularly the presence of the HLA-B27 gene, is strongly linked to reactive arthritis. However, not everyone with this gene will develop the condition.
- Age plays a role, as reactive arthritis most commonly affects individuals between the ages of 20 and 40.
- Gender differences are notable, with men being more likely to develop reactive arthritis following sexually transmitted infections, while women are more prone to cases triggered by gastrointestinal infections.
Symptoms of Reactive Arthritis
The symptoms of reactive arthritis can vary widely among individuals. They may appear suddenly or develop gradually over weeks. The condition typically manifests in three main areas: the joints, the urinary tract, and the eyes. However, not all patients experience symptoms in all three areas.
Joints
Joint pain and swelling are hallmark symptoms of reactive arthritis. The condition often affects the knees, ankles, and feet, but it can also involve the fingers, wrists, and shoulders. The affected joints may feel stiff, especially in the morning or after periods of inactivity. Unlike some forms of arthritis, reactive arthritis usually affects only one side of the body, leading to asymmetrical joint involvement.
Urinary Tract
Urinary symptoms are common in reactive arthritis and may include:
- Pain or burning during urination
- Frequent urge to urinate
- Inflammation of the urethra, known as urethritis
In some cases, men may experience swelling of the prostate gland, while women may develop inflammation of the cervix or fallopian tubes.
Eyes
Eye-related symptoms occur in approximately half of all individuals with reactive arthritis. These may include:
- Conjunctivitis, or redness and irritation of the eyes
- Uveitis, an inflammation of the middle layer of the eye, which can cause pain, sensitivity to light, and blurred vision
Skin and Other Symptoms
Some people with reactive arthritis may develop skin rashes, such as keratoderma blennorrhagica, which resembles psoriasis. Others may notice changes in their nails, such as pitting or thickening. Additional symptoms may include fatigue, fever, and weight loss.
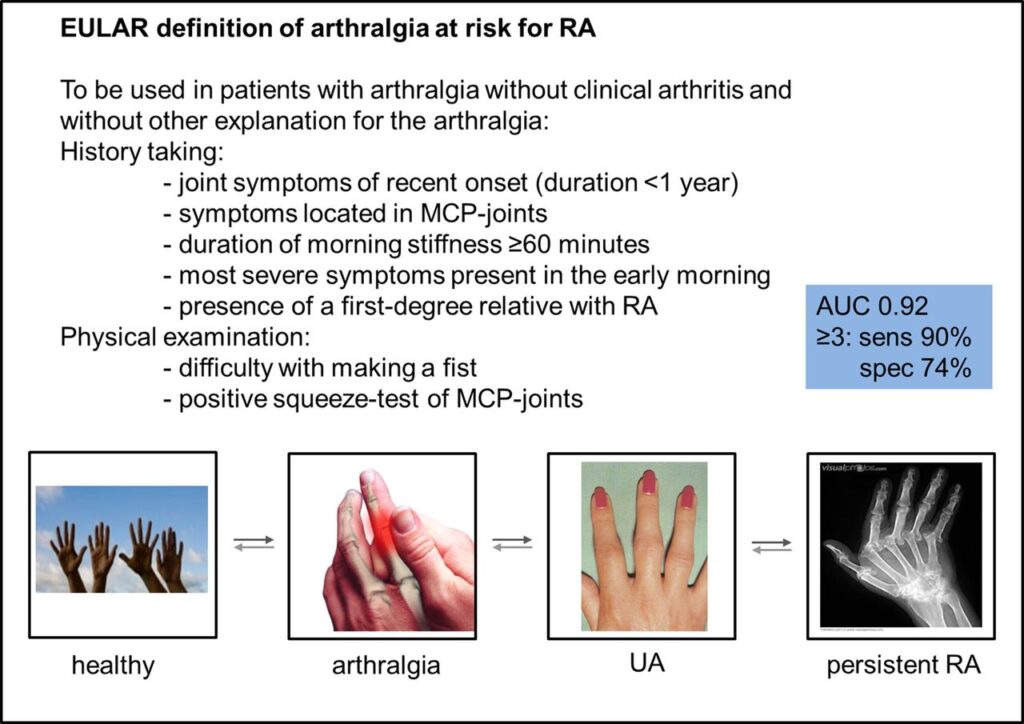
Diagnosing Reactive Arthritis
Diagnosing reactive arthritis can be challenging because its symptoms overlap with those of other conditions. There is no single test to confirm the presence of reactive arthritis, so healthcare providers rely on a combination of medical history, physical examination, laboratory tests, and imaging studies to make an accurate diagnosis.
Medical History and Physical Examination
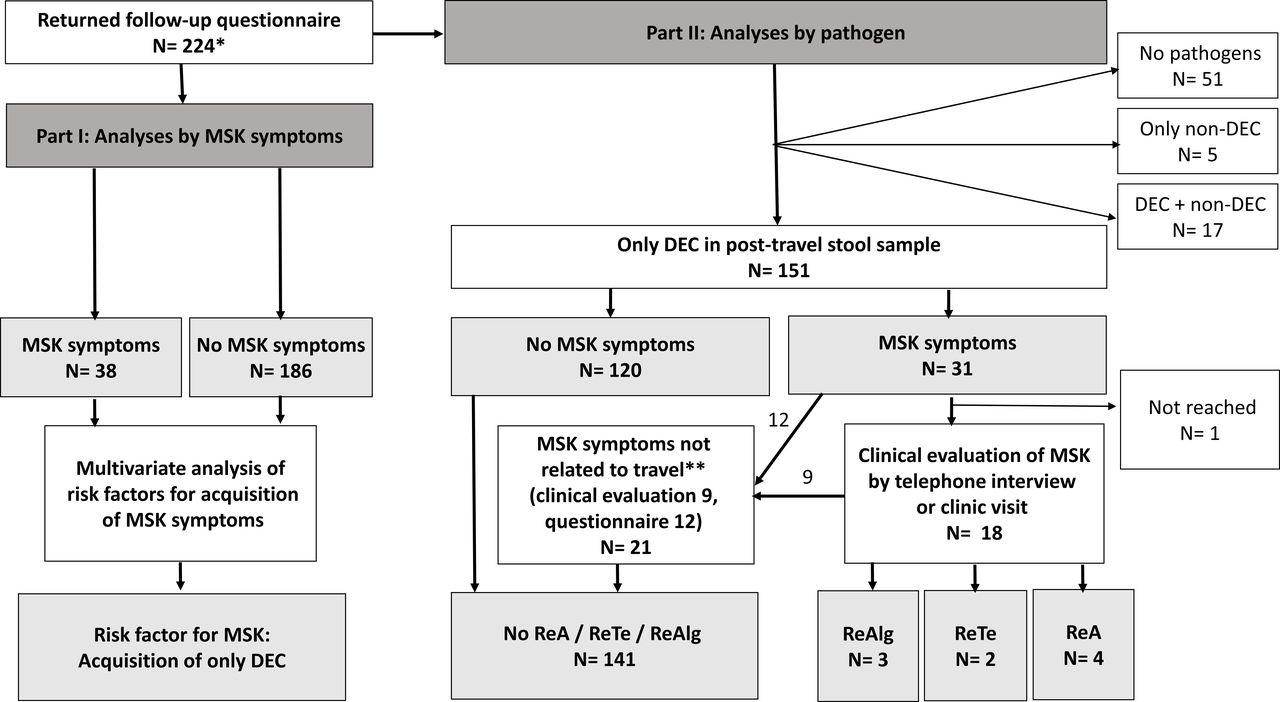
A thorough review of the patient’s medical history is crucial. The healthcare provider will ask about recent infections, sexual activity, travel history, and family history of arthritis or related conditions. During the physical examination, they will assess joint swelling, tenderness, and range of motion, as well as check for signs of eye inflammation or skin abnormalities.
Laboratory Tests
Blood tests are often used to support the diagnosis of reactive arthritis. These tests may include:
- Tests for markers of inflammation, such as C-reactive protein and erythrocyte sedimentation rate
- Tests for the presence of the HLA-B27 gene
- Cultures or tests to detect recent infections, such as stool samples for gastrointestinal pathogens or urine tests for sexually transmitted infections
Imaging Studies
X-rays and magnetic resonance imaging (MRI) scans may be used to evaluate joint damage or inflammation. Early in the disease, imaging results may appear normal, but over time, they can reveal characteristic changes, such as joint erosion or sacroiliitis (inflammation of the sacroiliac joints).
Treatment Options for Reactive Arthritis
While there is no cure for reactive arthritis, treatment focuses on managing symptoms, reducing inflammation, and preventing long-term complications. The approach to treatment depends on the severity of the condition and the specific symptoms experienced by the patient.
Medications
Several types of medications are commonly used to treat reactive arthritis:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These medications help reduce pain and inflammation. Over-the-counter options like ibuprofen and naproxen are often effective, but prescription-strength NSAIDs may be necessary for more severe cases.
- Corticosteroids: Injections of corticosteroids directly into the affected joints can provide rapid relief from inflammation. Oral corticosteroids may also be prescribed for widespread symptoms.
- Disease-Modifying Antirheumatic Drugs (DMARDs): For patients who do not respond to NSAIDs or corticosteroids, DMARDs such as sulfasalazine may be recommended. These medications work to slow the progression of the disease and protect the joints from damage.
- Antibiotics: If the underlying infection is caused by bacteria, antibiotics may be prescribed to eliminate the source of the infection. This is particularly important in cases triggered by sexually transmitted infections.
Physical Therapy
Physical therapy plays a vital role in maintaining joint function and improving flexibility. A physical therapist can design a personalized exercise program to strengthen the muscles around the affected joints, reduce stiffness, and enhance overall mobility. Stretching exercises, low-impact aerobic activities, and hydrotherapy are often included in the regimen.
Lifestyle Modifications
Making certain lifestyle changes can help manage symptoms and improve quality of life:
- Rest: Adequate rest is essential during flare-ups to allow the body to heal. However, prolonged inactivity should be avoided to prevent joint stiffness.
- Diet: A balanced diet rich in anti-inflammatory foods, such as fruits, vegetables, whole grains, and omega-3 fatty acids, can support overall health and reduce inflammation.
- Stress Management: Stress can exacerbate symptoms, so techniques such as meditation, yoga, and deep breathing exercises may be beneficial.
Monitoring and Follow-Up
Regular follow-up appointments with a healthcare provider are important to monitor the progression of the disease and adjust the treatment plan as needed. Patients should report any new or worsening symptoms promptly to ensure timely intervention.