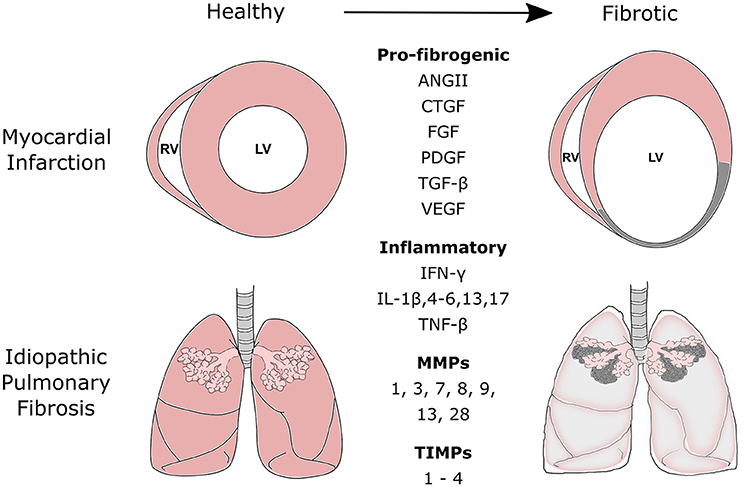
Pulmonary fibrosis, often abbreviated as PF, is a chronic and progressive lung disease that affects millions of people worldwide. It is characterized by the thickening and scarring of lung tissue, which leads to difficulty in breathing and reduced oxygen supply to the body. While the exact cause of this condition remains unknown in many cases, understanding its mechanisms, symptoms, diagnosis, and treatment options can help patients and caregivers navigate this challenging illness more effectively.
What is Pulmonary Fibrosis?
Pulmonary fibrosis refers to the abnormal formation of scar tissue within the lungs. This scarring disrupts the normal structure of the lung tissue, making it stiff and less elastic. As a result, the lungs lose their ability to expand and contract efficiently, leading to impaired gas exchange. Over time, this can severely impact a person’s quality of life and overall health.
The process of scarring in pulmonary fibrosis is often irreversible, meaning that once lung tissue becomes damaged, it cannot be repaired. However, early diagnosis and appropriate management can slow down the progression of the disease and improve symptoms.
Causes of Pulmonary Fibrosis
There are several potential causes of pulmonary fibrosis, though in many cases, the exact trigger remains unidentified. These causes can be broadly categorized into the following:
- Environmental Factors: Long-term exposure to pollutants, dust, or chemicals can irritate the lungs and lead to scarring. Occupations such as mining, farming, or construction may increase the risk due to prolonged inhalation of harmful substances.
- Medications: Certain drugs, including chemotherapy agents, antibiotics, and heart medications, have been linked to lung damage and subsequent scarring.
- Medical Conditions: Diseases such as rheumatoid arthritis, scleroderma, and sarcoidosis can contribute to the development of pulmonary fibrosis. These conditions are part of a group known as connective tissue disorders, which affect multiple organs, including the lungs.
- Unknown Causes: In some cases, no specific cause can be identified. This form of pulmonary fibrosis is referred to as idiopathic pulmonary fibrosis, which accounts for a significant proportion of cases.
Symptoms of Pulmonary Fibrosis
The symptoms of pulmonary fibrosis typically develop gradually and worsen over time. Some common signs include:
- Shortness of breath, especially during physical activity
- A persistent dry cough
- Fatigue and weakness
- Unexplained weight loss
- Clubbing of fingers or toes (a condition where the tips of the digits become rounded and enlarged)
As the disease progresses, individuals may experience shortness of breath even at rest, making daily activities increasingly difficult. Recognizing these symptoms early and seeking medical attention can make a significant difference in managing the condition.
Diagnosing Pulmonary Fibrosis
Diagnosing pulmonary fibrosis can be challenging because its symptoms often overlap with those of other respiratory conditions. A comprehensive evaluation is necessary to confirm the diagnosis, which may involve the following steps:
- Medical History and Physical Examination: The doctor will review the patient’s medical history, including any occupational exposures, medication use, and family history of lung diseases. A physical examination may reveal abnormal lung sounds, such as crackles.
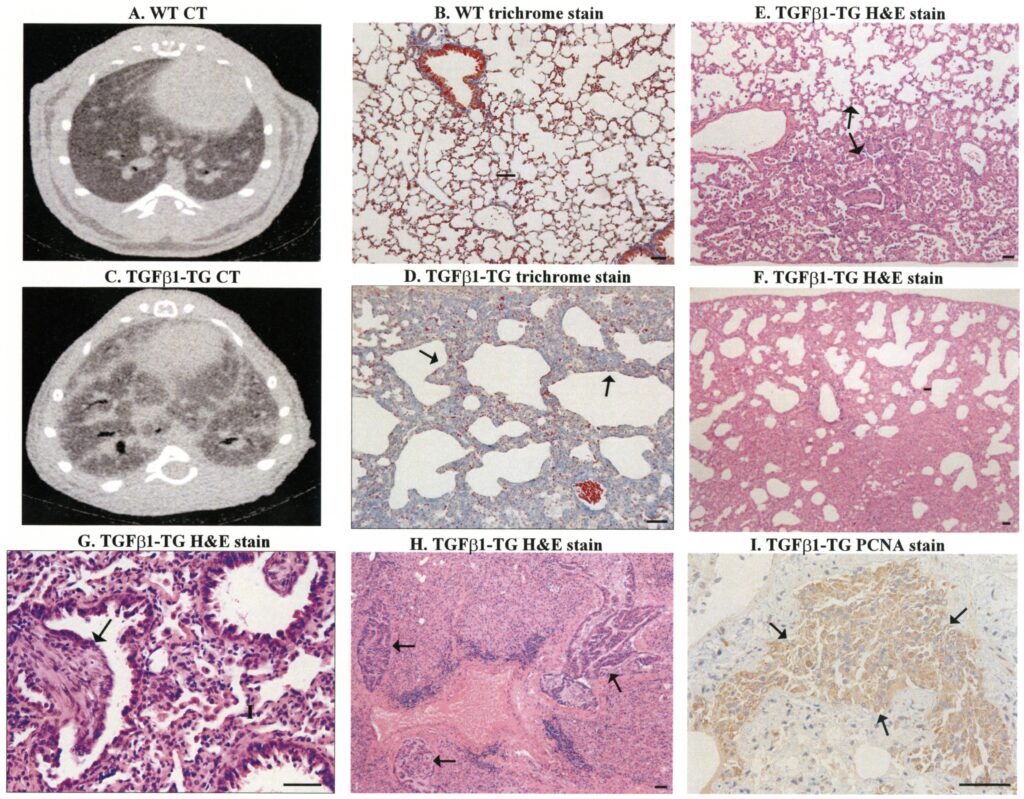
- Imaging Tests: High-resolution computed tomography scans of the chest are commonly used to visualize the extent of lung scarring. These images provide detailed information about the structure of the lungs and help differentiate pulmonary fibrosis from other conditions.
- Pulmonary Function Tests: These tests measure how well the lungs are functioning. They assess lung capacity, airflow, and the efficiency of oxygen transfer into the bloodstream.
- Laboratory Tests: Blood tests may be performed to rule out other diseases and identify markers associated with connective tissue disorders.
- Lung Biopsy: In some cases, a small sample of lung tissue may be removed for analysis. This procedure, although invasive, provides definitive evidence of scarring and helps determine the underlying cause.
Treatment Options for Pulmonary Fibrosis
While there is currently no cure for pulmonary fibrosis, various treatments aim to alleviate symptoms, slow disease progression, and improve quality of life. The choice of treatment depends on the severity of the condition and the individual’s overall health. Common approaches include:
- Medications: Antifibrotic drugs, such as pirfenidone and nintedanib, have been approved to slow the progression of idiopathic pulmonary fibrosis. Corticosteroids and immunosuppressants may also be prescribed to reduce inflammation and prevent further damage.
- Oxygen Therapy: Supplemental oxygen can help relieve shortness of breath and improve oxygen levels in the blood. This therapy is particularly beneficial for patients with advanced stages of the disease.
- Pulmonary Rehabilitation: This program combines exercise training, nutritional counseling, and education to enhance physical endurance and teach coping strategies. It empowers patients to manage their symptoms more effectively.
- Lifestyle Modifications: Quitting smoking, avoiding environmental irritants, and maintaining a healthy diet can support lung health and overall well-being.
- Lung Transplantation: For eligible candidates with severe pulmonary fibrosis, a lung transplant may be considered. This surgical procedure replaces damaged lungs with healthy donor lungs, offering a chance for improved survival and quality of life.
Living with Pulmonary Fibrosis
Managing pulmonary fibrosis requires a multidisciplinary approach involving healthcare providers, patients, and their families. Emotional and psychological support is equally important, as living with a chronic illness can take a toll on mental health. Support groups, counseling, and educational resources can provide valuable assistance in coping with the challenges of the disease.
Patients are encouraged to stay proactive in their care by adhering to treatment plans, attending regular follow-ups, and reporting any new or worsening symptoms promptly. Additionally, staying informed about advancements in research and treatment options can offer hope and empower individuals to make informed decisions about their health.
Research and Future Directions
Ongoing research is focused on unraveling the mysteries of pulmonary fibrosis and developing innovative therapies. Scientists are exploring the role of genetics, immune system dysfunction, and cellular pathways in the development of the disease. Promising areas of investigation include stem cell therapy, gene editing, and targeted drug delivery systems.
Clinical trials play a crucial role in advancing our understanding of pulmonary fibrosis and testing new treatments. Patients who participate in these studies contribute to the collective effort to find better solutions for managing and potentially curing this debilitating condition.
Preventing Pulmonary Fibrosis
While not all cases of pulmonary fibrosis can be prevented, certain measures can reduce the risk of developing the disease or slow its progression:
- Avoid exposure to harmful substances, such as asbestos, silica, and tobacco smoke.
- Use protective equipment when working in environments with high levels of dust or chemicals.
- Seek prompt treatment for respiratory infections and other lung-related issues.
- Maintain a healthy lifestyle, including regular exercise and a balanced diet.
By adopting these preventive strategies, individuals can safeguard their lung health and minimize the likelihood of developing pulmonary fibrosis.