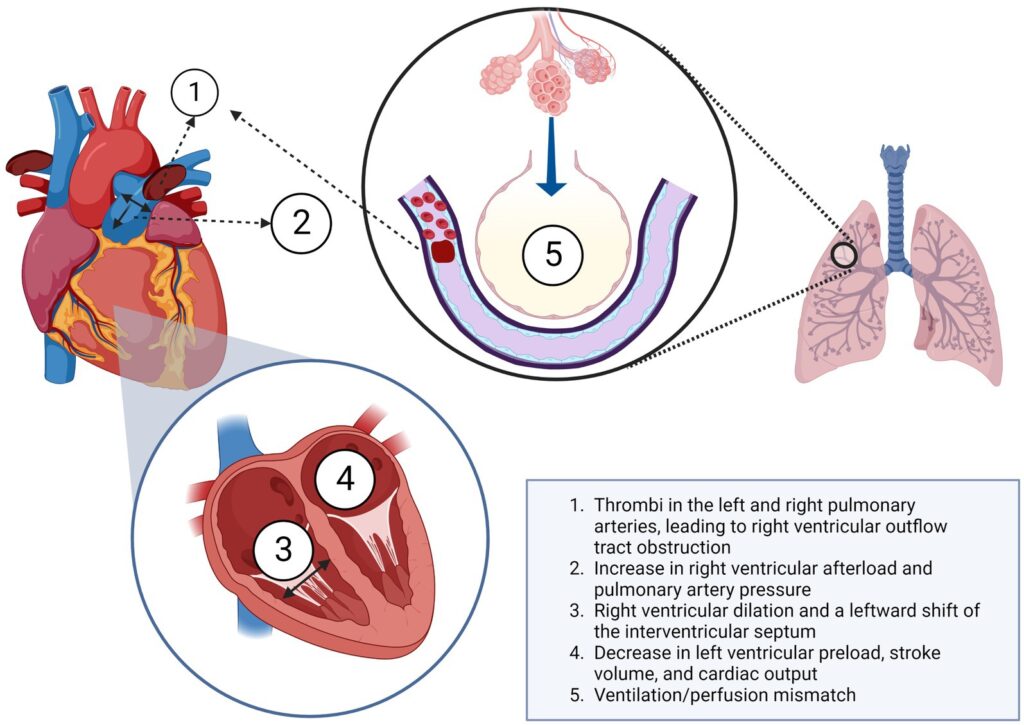
A pulmonary embolism (PE) is a serious medical condition that occurs when a blood clot travels to the lungs, blocking one of the pulmonary arteries. This blockage can severely affect breathing and other vital functions of the body. If left untreated, it can lead to life-threatening complications. Understanding its causes, recognizing its symptoms, and knowing how it is diagnosed and treated are crucial for managing this condition effectively.
What Causes Pulmonary Embolism?
The primary cause of pulmonary embolism is the formation of blood clots, most commonly in the deep veins of the legs. This condition is known as deep vein thrombosis. When a piece of the clot breaks loose, it travels through the bloodstream and eventually reaches the lungs, where it becomes lodged in a pulmonary artery. Several factors increase the risk of developing these clots:
- Prolonged Immobility: Long periods of inactivity, such as during extended travel or bed rest after surgery, can slow blood flow in the veins, increasing the likelihood of clot formation.
- Surgical Procedures: Surgeries, especially those involving the hips, knees, or abdomen, pose a higher risk of blood clots due to tissue trauma and reduced mobility post-operation.
- Medical Conditions: Certain health issues, including cancer, heart disease, and autoimmune disorders, can make the blood more prone to clotting.
- Hormonal Factors: The use of oral contraceptives or hormone replacement therapy, as well as pregnancy, can elevate the risk of clot formation due to hormonal changes.
- Obesity: Excess weight puts additional pressure on the veins in the pelvis and legs, making them more susceptible to clot formation.
- Smoking: Smoking damages blood vessels and increases the risk of clot formation by affecting circulation and blood chemistry.
Recognizing the Symptoms of Pulmonary Embolism
The symptoms of pulmonary embolism can vary depending on the size of the clot and the portion of the lung affected. In some cases, individuals may not experience any noticeable symptoms, while others may exhibit severe signs that require immediate medical attention. Common symptoms include:
- Sudden Shortness of Breath: Difficulty breathing often occurs suddenly and worsens with exertion. It is one of the hallmark signs of this condition.
- Chest Pain: Sharp or stabbing pain in the chest may occur, which can feel worse when taking deep breaths, coughing, or bending over.
- Rapid Heart Rate: An increased heart rate, also known as tachycardia, is a common symptom as the heart works harder to compensate for reduced oxygen levels in the blood.
- Coughing: Some individuals may develop a persistent cough, which may produce bloody or blood-streaked sputum.
- Lightheadedness or Fainting: A sudden drop in blood pressure caused by the blockage can lead to dizziness, fainting, or even loss of consciousness.
- Anxiety or Restlessness: Many people report feelings of unease or panic, which may be linked to difficulty breathing and chest discomfort.
In severe cases, a large clot can cause significant damage to the lungs and other organs due to lack of oxygen, leading to life-threatening complications such as cardiac arrest.
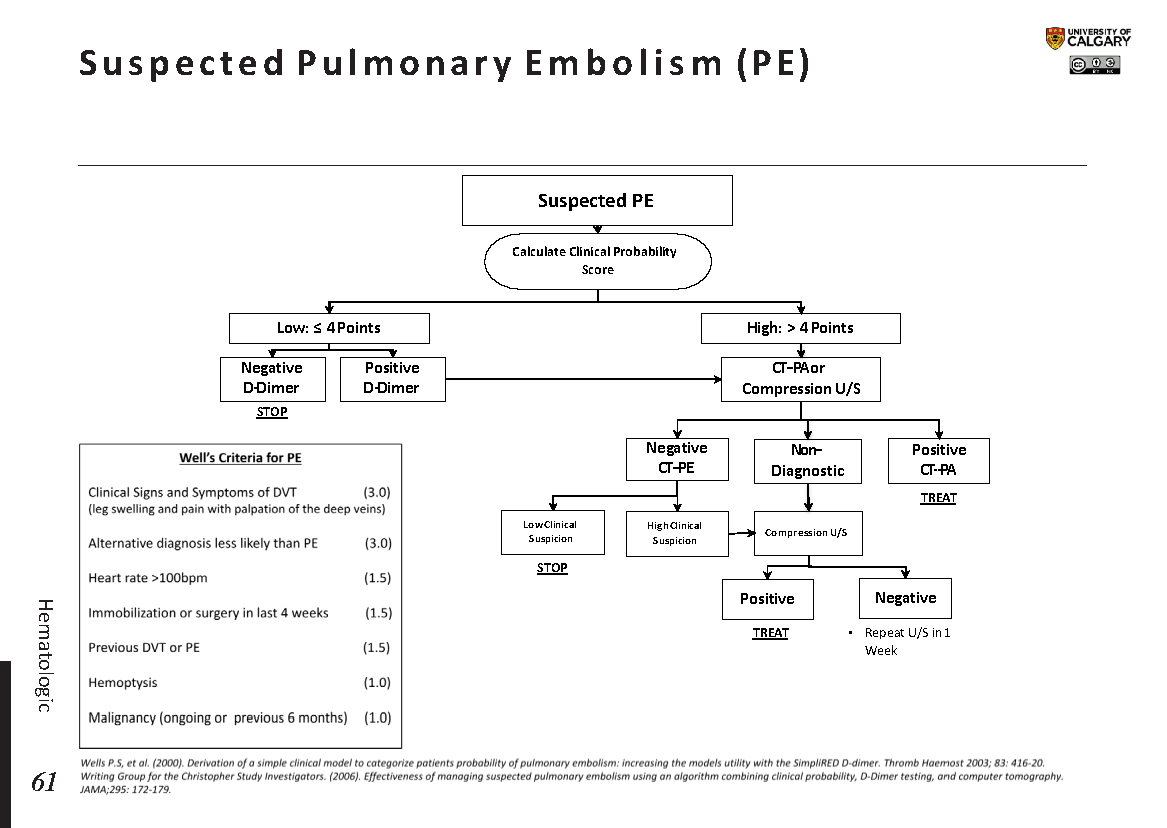
How is Pulmonary Embolism Diagnosed?
Diagnosing pulmonary embolism can be challenging because its symptoms often mimic those of other conditions, such as heart attacks, pneumonia, or panic attacks. To confirm the presence of a blood clot in the lungs, healthcare providers typically rely on a combination of clinical evaluation and diagnostic tests.
Initial Assessment
During the initial assessment, a doctor will review the patient’s medical history, perform a physical examination, and ask about symptoms. They may inquire about recent surgeries, prolonged immobility, family history of blood clots, or underlying health conditions that could increase the risk of clot formation.
Imaging Tests
Several imaging tests are used to visualize the lungs and identify potential blockages:
- Computed Tomography Pulmonary Angiography: This is the most common test used to diagnose pulmonary embolism. It involves injecting a contrast dye into the bloodstream and using CT scans to create detailed images of the blood vessels in the lungs.
- Ventilation-Perfusion Scan: Also known as a VQ scan, this test measures airflow and blood flow in the lungs. Areas with normal airflow but poor blood flow may indicate a blockage.
- Chest X-Ray: While not definitive for diagnosing pulmonary embolism, a chest X-ray can help rule out other conditions, such as pneumonia or fluid around the lungs.
Blood Tests
Blood tests play an important role in confirming the diagnosis:
- D-Dimer Test: This test measures a substance released when a blood clot breaks down. Elevated levels suggest the presence of a clot, although they can also be elevated in other conditions.
- Arterial Blood Gas Analysis: This test measures the levels of oxygen and carbon dioxide in the blood, helping to assess how well the lungs are functioning.
Treatment Options for Pulmonary Embolism
The treatment of pulmonary embolism focuses on preventing the clot from growing larger, reducing the risk of new clots, and managing symptoms. The specific approach depends on the severity of the condition and the patient’s overall health.
Anticoagulant Medications
Anticoagulants, also known as blood thinners, are the first line of treatment for most cases of pulmonary embolism. These medications do not dissolve existing clots but prevent them from enlarging and reduce the risk of additional clots forming. Commonly prescribed anticoagulants include:
- Heparin: Administered intravenously or via injection, heparin works quickly to prevent further clot formation.
- Warfarin: Taken orally, warfarin requires regular monitoring of blood levels to ensure the dosage remains effective.
- Direct Oral Anticoagulants: These newer medications, such as rivaroxaban and apixaban, offer the convenience of oral administration without the need for frequent monitoring.
Thrombolytic Therapy
In severe cases where the clot is large and poses an immediate threat to life, thrombolytic medications may be used. These drugs, also called clot busters, work by dissolving the clot rapidly. However, they carry a higher risk of bleeding and are typically reserved for critical situations.
Inferior Vena Cava Filters
For patients who cannot take anticoagulants due to a high risk of bleeding, an inferior vena cava filter may be inserted. This small device is placed in the largest vein in the abdomen to trap clots before they reach the lungs.
Oxygen Therapy
If low oxygen levels are detected, supplemental oxygen may be administered to improve breathing and ensure adequate oxygen supply to the body’s tissues.
Surgical Intervention
In rare cases, surgical procedures such as embolectomy may be performed to remove the clot directly from the pulmonary artery. This option is considered only when other treatments have failed or are contraindicated.
Lifestyle Modifications
After the acute phase of treatment, lifestyle changes can help reduce the risk of future clots:
- Regular Exercise: Staying active improves circulation and reduces the risk of clot formation.
- Healthy Diet: A balanced diet rich in fruits, vegetables, and whole grains supports overall cardiovascular health.
- Weight Management: Maintaining a healthy weight alleviates pressure on the veins and lowers the risk of clot-related complications.
- Avoiding Smoking: Quitting smoking improves blood vessel health and reduces clotting risks.
Preventing Recurrence of Pulmonary Embolism
Once a person has experienced a pulmonary embolism, they are at an increased risk of developing another clot. Preventive measures are essential to minimize this risk:
- Long-Term Anticoagulation: Many patients are prescribed blood thinners for several months or even indefinitely, depending on their individual risk factors.
- Compression Stockings: Wearing graduated compression stockings can improve blood flow in the legs and reduce the risk of deep vein thrombosis.
- Regular Follow-Up: Routine check-ups with a healthcare provider allow for ongoing monitoring and adjustment of treatment plans as needed.
By understanding the causes, recognizing the symptoms, and adhering to prescribed treatments, individuals can effectively manage pulmonary embolism and reduce the likelihood of recurrence.