Psoriasis, often abbreviated as Pso, is a chronic autoimmune condition that affects millions of people worldwide. It manifests as patches of red, inflamed skin covered with silvery scales, causing discomfort and impacting the quality of life for those who live with it. While there is no cure for this condition, understanding its causes, triggers, and available treatments can empower individuals to manage their symptoms effectively. This article delves into the intricacies of psoriasis, exploring its underlying mechanisms, common triggers, and the diverse range of treatment options available.
What Is Psoriasis?
Psoriasis is a non-contagious skin disorder characterized by the rapid buildup of skin cells. Normally, skin cells grow and shed in a cycle that lasts about a month. However, in individuals with psoriasis, this process accelerates, taking only a few days. The result is an accumulation of cells on the surface of the skin, forming thick, scaly patches known as plaques. These plaques can appear anywhere on the body but are most commonly found on the elbows, knees, scalp, and lower back.
There are several types of psoriasis, each with distinct characteristics:
- Plaque Psoriasis: The most common form, marked by raised, red patches covered with a silvery-white buildup of dead skin cells.
- Guttate Psoriasis: Small, dot-like lesions that often appear after a bacterial infection, such as strep throat.
- Inverse Psoriasis: Smooth, red patches that develop in skin folds, such as the armpits or groin.
- Pustular Psoriasis: White blisters surrounded by red skin, typically occurring on the hands and feet.
- Erythrodermic Psoriasis: A rare and severe form that causes widespread redness and shedding of the skin.
The Science Behind Psoriasis
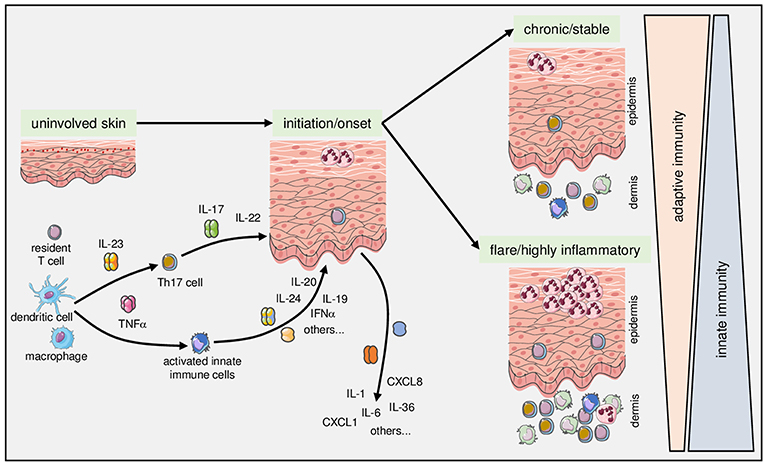
At its core, psoriasis is an immune-mediated condition. This means that the immune system mistakenly attacks healthy skin cells, triggering inflammation and accelerating the skin cell production process. Researchers believe that both genetic and environmental factors play a role in the development of psoriasis. While the exact cause remains unknown, certain genes have been identified as contributing to the risk of developing the condition.
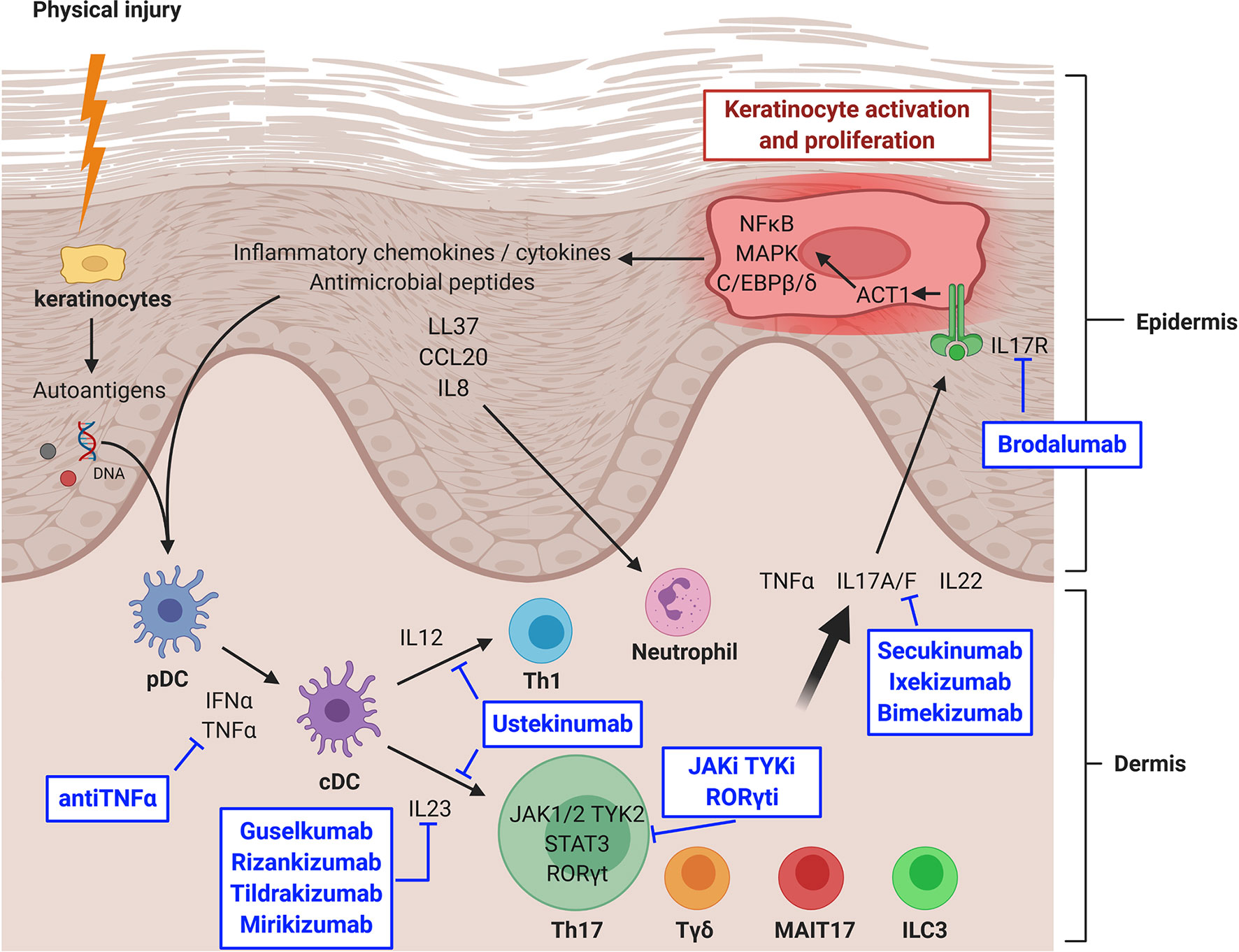
One key player in psoriasis is a type of white blood cell called a T-cell. In individuals without psoriasis, T-cells help protect the body from infections. However, in those with psoriasis, T-cells become overactive and attack healthy skin cells by mistake. This immune response leads to increased production of new skin cells, more T-cells, and other inflammatory cells, creating a cycle of inflammation and skin cell buildup.
Genetic Factors
Family history is a significant risk factor for psoriasis. If one parent has the condition, the child has a higher likelihood of developing it. If both parents have psoriasis, the risk increases further. Despite this, not everyone with a genetic predisposition will develop the condition, suggesting that environmental triggers also play a crucial role.
Environmental Triggers
While genetics lay the groundwork for psoriasis, environmental factors often act as triggers that bring the condition to the surface. Identifying and avoiding these triggers can help manage symptoms and reduce flare-ups. Common triggers include:
- Stress: Emotional stress can exacerbate psoriasis by weakening the immune system and increasing inflammation.
- Infections: Bacterial or viral infections, such as strep throat or respiratory infections, can trigger guttate psoriasis or worsen existing symptoms.
- Injuries to the Skin: Cuts, scrapes, bug bites, or even excessive scratching can lead to the development of new psoriasis plaques in a phenomenon known as the Koebner effect.
- Medications: Certain medications, including lithium, beta-blockers, and antimalarial drugs, may trigger or worsen psoriasis.
- Weather Changes: Cold, dry weather can dry out the skin and worsen symptoms, while warm, sunny weather often provides relief.
- Smoking and Alcohol: Both smoking and excessive alcohol consumption have been linked to an increased risk of developing psoriasis and worsening its severity.
Treatment Options for Psoriasis
Although psoriasis cannot be cured, a variety of treatments are available to help manage symptoms and improve the quality of life for those affected. Treatment plans are highly individualized, depending on the type and severity of psoriasis, as well as the patient’s overall health and lifestyle. Below are the main categories of treatment options:
Topical Treatments
Topical treatments are applied directly to the skin and are often the first line of defense for mild to moderate psoriasis. These treatments aim to reduce inflammation, slow down skin cell growth, and alleviate itching. Common topical treatments include:
- Corticosteroids: These anti-inflammatory medications help reduce redness and swelling. They come in various strengths and are typically used for short periods to avoid side effects like skin thinning.
- Vitamin D Analogues: Synthetic forms of vitamin D help slow skin cell growth and are often used in combination with corticosteroids.
- Retinoids: Derived from vitamin A, these medications normalize DNA activity in skin cells and reduce inflammation.
- Salicylic Acid: This ingredient helps remove dead skin cells and reduce scaling.
- Coal Tar: A traditional treatment that reduces scaling, itching, and inflammation. However, it can be messy and has a strong odor.
Phototherapy
Phototherapy, also known as light therapy, involves exposing the skin to ultraviolet light under medical supervision. This treatment slows down the growth of skin cells and reduces inflammation. There are two primary types of phototherapy:
- UVB Phototherapy: Uses ultraviolet B light to target affected areas of the skin. It is effective for mild to moderate psoriasis.
- Puva Therapy: Combines exposure to ultraviolet A light with a medication called psoralen, which makes the skin more sensitive to light.
Systemic Medications
For moderate to severe psoriasis that does not respond to topical treatments or phototherapy, systemic medications may be prescribed. These medications work throughout the body and are administered orally or via injection. Examples include:
- Methotrexate: An immunosuppressant that slows skin cell turnover and reduces inflammation.
- Cyclosporine: Suppresses the immune system to prevent it from attacking healthy skin cells.
- Biologics: Target specific parts of the immune system involved in psoriasis. These include tumor necrosis factor-alpha inhibitors, interleukin inhibitors, and others.
Lifestyle Modifications
In addition to medical treatments, making certain lifestyle changes can help manage psoriasis symptoms. These include:
- Moisturizing Regularly: Keeping the skin hydrated can reduce dryness and scaling.
- Avoiding Triggers: Identifying and avoiding personal triggers can prevent flare-ups.
- Eating a Balanced Diet: Some studies suggest that diets rich in anti-inflammatory foods, such as fruits, vegetables, and omega-3 fatty acids, may help reduce symptoms.
- Managing Stress: Techniques like meditation, yoga, and deep breathing can help reduce stress levels and minimize flare-ups.
Living with Psoriasis
Psoriasis is more than just a skin condition; it can significantly impact mental health and emotional well-being. Many individuals with psoriasis experience feelings of embarrassment, anxiety, or depression due to the visible nature of the condition. Seeking support from healthcare providers, joining support groups, and connecting with others who understand the challenges of living with psoriasis can make a profound difference.
Education is also a powerful tool. By learning about the condition, its triggers, and available treatments, individuals can take an active role in managing their health. Regular communication with dermatologists and other healthcare professionals ensures that treatment plans remain effective and up-to-date.
Emerging Research and Future Directions
Research into psoriasis is ongoing, with scientists continually exploring new treatments and potential cures. Advances in biologic therapies, gene therapy, and personalized medicine hold promise for more targeted and effective treatments in the future. Additionally, a deeper understanding of the relationship between psoriasis and other conditions, such as psoriatic arthritis and cardiovascular disease, is helping to improve holistic care for patients.