Pseudogout, also known as Calcium Pyrophosphate Deposition Disease or CPPD, is a type of arthritis that occurs when calcium pyrophosphate crystals accumulate in the joints. These crystal deposits lead to sudden and painful inflammation, often mimicking the symptoms of gout. However, unlike gout, which is caused by uric acid crystals, pseudogout involves a different type of crystal. In this article, we will explore the causes, symptoms, diagnosis, and treatment options for this condition.
What Causes Pseudogout?
The exact cause of pseudogout remains unclear, but several factors are believed to contribute to its development. Understanding these factors can help in managing and preventing the condition.
Age
Pseudogout is more common in older adults, particularly those over the age of 60. As people age, the cartilage in their joints naturally begins to break down, creating an environment where calcium pyrophosphate crystals can form and accumulate.
Genetic Factors
Some individuals may have a genetic predisposition to developing pseudogout. Mutations in certain genes that regulate the metabolism of calcium and other minerals can increase the likelihood of crystal formation in the joints.
Underlying Health Conditions
- Hyperparathyroidism: This condition causes excessive production of parathyroid hormone, leading to elevated levels of calcium in the blood, which can promote crystal formation.
- Hemochromatosis: A disorder characterized by excessive iron storage in the body, hemochromatosis can damage joint tissues and create conditions favorable for crystal deposition.
- Hypothyroidism: Low thyroid function has been associated with an increased risk of pseudogout due to its impact on calcium regulation.
- Kidney Disease: Impaired kidney function can disrupt the balance of minerals in the body, contributing to the development of calcium pyrophosphate crystals.
Injury or Surgery
Trauma to a joint, such as a fracture or surgery, can trigger an inflammatory response that may lead to the deposition of calcium pyrophosphate crystals. This is why pseudogout sometimes occurs after joint-related procedures.
Symptoms of Pseudogout
The symptoms of pseudogout can vary from person to person, but they often resemble those of other types of arthritis, making accurate diagnosis crucial.
Sudden Joint Pain
One of the hallmark symptoms of pseudogout is sudden and intense pain in one or more joints. The knees are most commonly affected, but other joints such as the wrists, shoulders, and ankles can also be involved. The pain typically comes on quickly and may last for several days or weeks.
Swelling and Redness
Along with pain, the affected joint may become swollen, warm, and red. This inflammation is a result of the body’s immune response to the presence of calcium pyrophosphate crystals in the joint.
Stiffness and Reduced Mobility
Individuals with pseudogout often experience stiffness in the affected joint, especially in the morning or after periods of inactivity. This stiffness can limit mobility and make it difficult to perform daily activities.
Chronic Joint Damage
If left untreated, repeated episodes of pseudogout can lead to chronic joint damage. Over time, the accumulation of calcium pyrophosphate crystals can erode cartilage and cause degenerative changes similar to osteoarthritis.
Diagnosing Pseudogout
Diagnosing pseudogout requires a combination of clinical evaluation, imaging studies, and laboratory tests. Since the symptoms of pseudogout overlap with other forms of arthritis, a thorough diagnostic process is essential.
Medical History and Physical Examination
A healthcare provider will begin by taking a detailed medical history and performing a physical examination. They will ask about the onset, duration, and severity of symptoms, as well as any underlying health conditions or family history of arthritis.
Joint Fluid Analysis
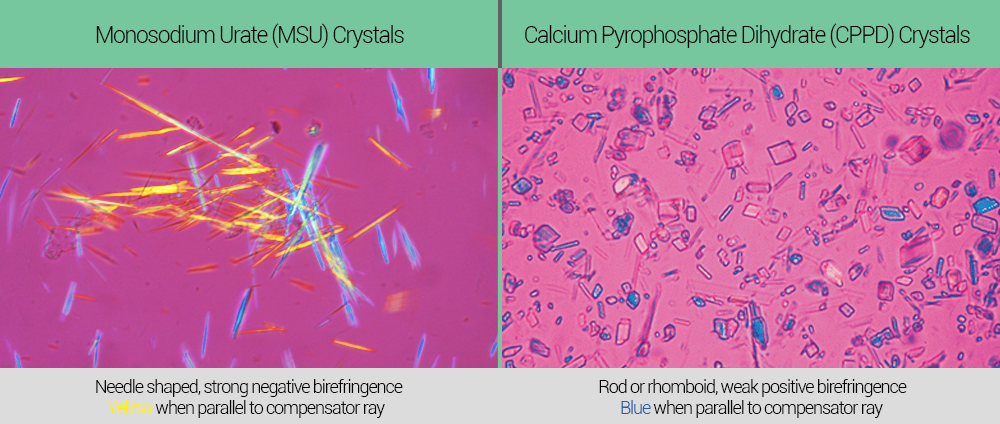
To confirm the presence of calcium pyrophosphate crystals, a sample of fluid from the affected joint may be extracted using a needle. This procedure, called arthrocentesis, allows doctors to examine the fluid under a microscope. The identification of rhomboid-shaped crystals confirms the diagnosis of pseudogout.
Imaging Studies
X-rays are often used to detect calcium pyrophosphate deposits in the joints. These deposits appear as white spots on the images and are a key indicator of the disease. In some cases, ultrasound or magnetic resonance imaging may also be used to assess joint damage and inflammation.
Blood Tests
While blood tests cannot directly diagnose pseudogout, they can help rule out other conditions such as gout or rheumatoid arthritis. Blood tests may measure levels of uric acid, calcium, and other markers of inflammation.
Treatment Options for Pseudogout
Although there is no cure for pseudogout, various treatments can help manage symptoms and prevent future flare-ups. The choice of treatment depends on the severity of the condition and the individual’s overall health.
Medications
Several types of medications are commonly used to treat pseudogout:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These medications, such as ibuprofen and naproxen, are often the first line of treatment for mild to moderate pseudogout. They help reduce pain and inflammation.
- Colchicine: Originally used to treat gout, colchicine can also be effective in managing acute attacks of pseudogout. It works by reducing inflammation and preventing crystal-induced damage.
- Corticosteroids: For individuals who cannot take NSAIDs or colchicine, corticosteroid injections into the affected joint may provide rapid relief from pain and swelling.
Lifestyle Modifications
Making certain lifestyle changes can help manage pseudogout and improve overall joint health:
- Dietary Adjustments: While diet does not directly cause pseudogout, maintaining a balanced diet rich in anti-inflammatory foods can support joint health. Foods high in omega-3 fatty acids, such as fish and flaxseeds, may be particularly beneficial.
- Weight Management: Excess weight puts additional stress on the joints, increasing the risk of inflammation and damage. Losing weight can alleviate pressure on the joints and reduce the frequency of flare-ups.
- Exercise: Low-impact exercises like swimming, walking, and yoga can improve joint flexibility and strengthen supporting muscles without causing further damage.
Joint Aspiration
In cases of severe swelling, joint aspiration may be performed to remove excess fluid from the affected joint. This procedure not only provides immediate relief but also allows for analysis of the joint fluid to confirm the presence of calcium pyrophosphate crystals.
Surgery
In rare cases where pseudogout leads to significant joint damage, surgical intervention may be necessary. Procedures such as joint replacement surgery can restore function and alleviate chronic pain.
Preventing Future Flare-Ups
While it may not be possible to completely prevent pseudogout, certain strategies can reduce the risk of future flare-ups:
- Regular Monitoring: Individuals with a history of pseudogout should have regular check-ups with their healthcare provider to monitor joint health and address any early signs of inflammation.
- Managing Underlying Conditions: Properly managing conditions like hyperparathyroidism, hemochromatosis, or hypothyroidism can help minimize the risk of crystal formation.
- Staying Hydrated: Drinking plenty of water helps maintain healthy mineral balance in the body, potentially reducing the likelihood of crystal deposits.
Living with Pseudogout
Living with pseudogout requires a proactive approach to managing symptoms and maintaining joint health. By working closely with healthcare providers and adopting healthy lifestyle habits, individuals with this condition can lead active and fulfilling lives despite the challenges posed by the disease.





