Prostatitis, often abbreviated as PT, is a condition that affects the prostate gland, leading to inflammation and discomfort. This condition can significantly impact a man’s quality of life, causing pain and urinary problems. In this article, we will explore the causes, symptoms, diagnosis methods, and treatment options available for prostatitis.
What is Prostatitis?
Prostatitis refers to the inflammation or infection of the prostate gland, which is located below the bladder in men. The prostate plays a crucial role in reproductive health by producing fluid that nourishes and transports sperm. When this gland becomes inflamed, it can lead to various symptoms that affect urinary and sexual functions.
Types of Prostatitis
- Acute Bacterial Prostatitis: This type is caused by a bacterial infection and develops suddenly. It is often accompanied by severe symptoms.
- Chronic Bacterial Prostatitis: A recurring bacterial infection of the prostate gland that persists over time.
- Chronic Pelvic Pain Syndrome: Also known as nonbacterial prostatitis, this is the most common form and does not involve a bacterial infection.
- Asymptomatic Inflammatory Prostatitis: This type does not present noticeable symptoms but may be detected during medical examinations for other conditions.
Causes of Prostatitis
The exact cause of prostatitis varies depending on the type. Understanding these causes is essential for proper diagnosis and treatment.
Bacterial Infections
Acute and chronic bacterial prostatitis are primarily caused by bacterial infections. These bacteria can enter the prostate through the urethra, which is the tube that carries urine out of the body. Common bacteria responsible include Escherichia coli and Klebsiella pneumoniae. Factors such as urinary tract infections, sexually transmitted infections, and catheter use can increase the risk of bacterial prostatitis.
Nonbacterial Causes
Chronic pelvic pain syndrome, the most common form of prostatitis, does not involve bacterial infections. Instead, it may result from immune system disorders, nerve damage in the pelvic area, or pressure on the prostate from nearby muscles or bones. Stress and anxiety can also contribute to the development of this condition.
Risk Factors
Certain factors can increase the likelihood of developing prostatitis:
- A history of urinary tract infections
- Engaging in unprotected sexual activity
- Having a compromised immune system
- Using urinary catheters frequently
- Experiencing trauma or injury to the pelvic region
Symptoms of Prostatitis
The symptoms of prostatitis can vary depending on the type and severity of the condition. Some men experience mild discomfort, while others face debilitating pain and dysfunction.
Urinary Symptoms
One of the hallmark signs of prostatitis is difficulty with urination. Common urinary symptoms include:
- Frequent urge to urinate
- Pain or burning sensation during urination
- Difficulty starting or stopping the urine stream
- Weak urine flow
- Dribbling after urination
Pain and Discomfort
Pain is another prominent symptom of prostatitis. It can manifest in various areas of the body, including:
- The perineum (the area between the scrotum and anus)
- The lower back
- The groin
- The penis or testicles
Sexual Dysfunction
Some men with prostatitis may experience issues related to sexual health, such as:
- Pain during or after ejaculation
- Erectile dysfunction
- Decreased libido
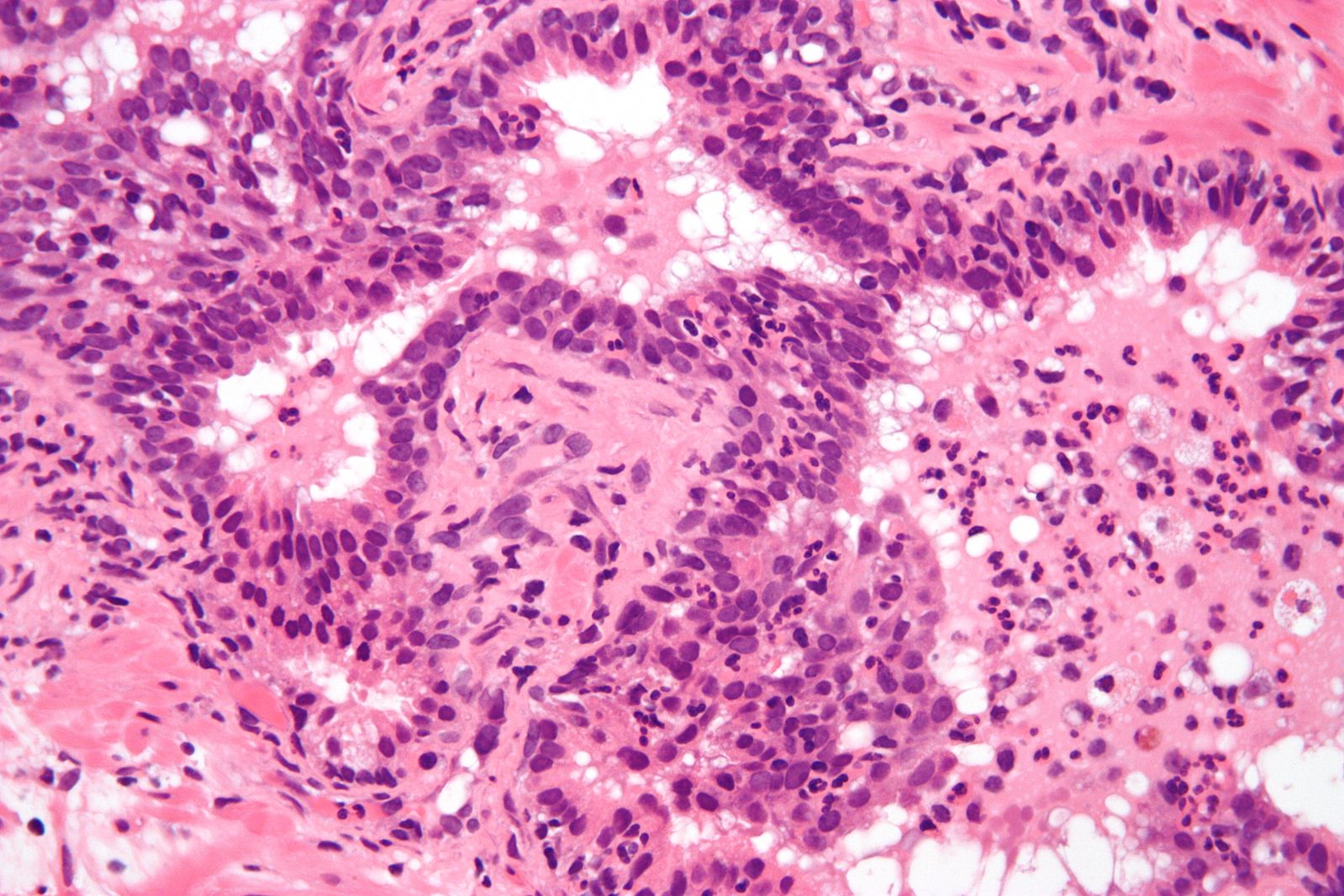
Diagnosis of Prostatitis
Diagnosing prostatitis requires a thorough evaluation by a healthcare professional. Since the symptoms of prostatitis can mimic those of other conditions, accurate diagnosis is critical for effective treatment.
Medical History and Physical Examination
The first step in diagnosing prostatitis involves taking a detailed medical history and conducting a physical examination. During the physical exam, the doctor may perform a digital rectal examination to assess the size, shape, and texture of the prostate gland.
Urine and Blood Tests
Urine and blood tests are commonly used to check for signs of infection or inflammation. A urine culture can help identify the presence of bacteria, while blood tests may reveal elevated white blood cell counts, indicating an infection.
Prostate Fluid Analysis
In some cases, the doctor may massage the prostate to collect a sample of prostate fluid. This fluid is then analyzed for signs of infection or inflammation.
Imaging Tests
Imaging tests, such as ultrasound or magnetic resonance imaging, may be used to visualize the prostate and surrounding structures. These tests can help rule out other conditions, such as prostate cancer or bladder disorders.
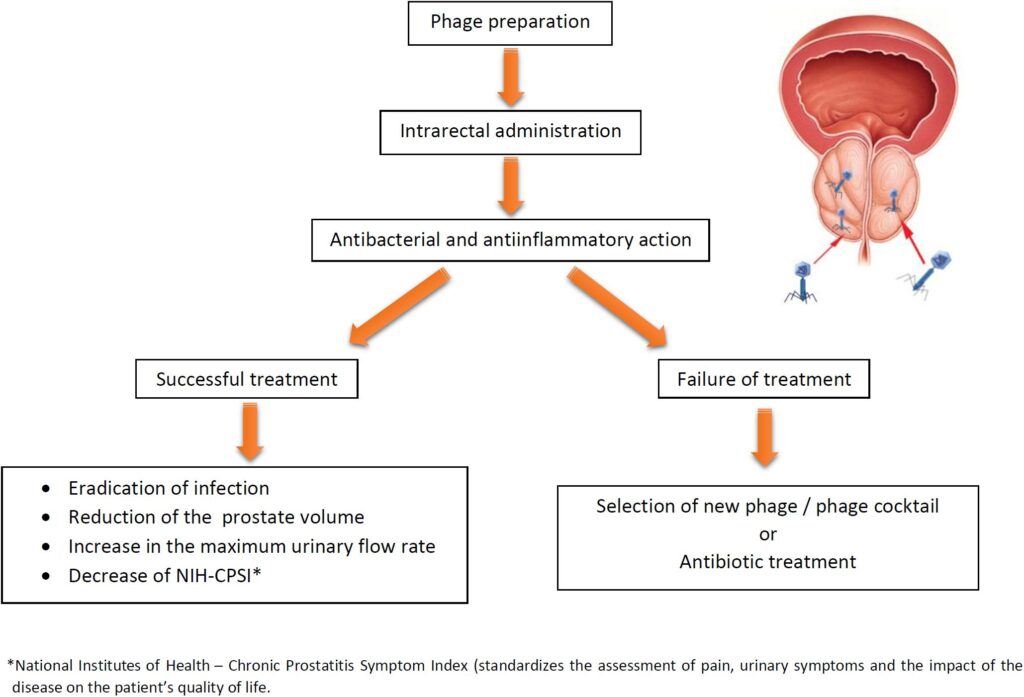
Treatment Options for Prostatitis
The treatment of prostatitis depends on the underlying cause and the type of prostatitis. While some cases can be managed with medication, others may require a combination of therapies.
Antibiotics
For bacterial prostatitis, antibiotics are the primary treatment. The choice of antibiotic and the duration of treatment depend on the specific bacteria causing the infection. Commonly prescribed antibiotics include fluoroquinolones and trimethoprim-sulfamethoxazole. In chronic cases, treatment may last several weeks or even months.
Alpha-Blockers
Alpha-blockers are medications that relax the muscles in the prostate and bladder neck, improving urine flow and reducing symptoms. These medications are often used in conjunction with antibiotics for chronic prostatitis.
Anti-Inflammatory Medications
Nonsteroidal anti-inflammatory drugs, such as ibuprofen, can help reduce pain and inflammation associated with prostatitis. These medications are particularly useful for managing symptoms of chronic pelvic pain syndrome.
Heat Therapy
Applying heat to the pelvic area can provide relief from pain and discomfort. Warm baths or heating pads are simple yet effective ways to alleviate symptoms.
Lifestyle Modifications
Making certain lifestyle changes can also help manage prostatitis symptoms:
- Drinking plenty of water to flush out bacteria
- Avoiding caffeine, alcohol, and spicy foods that irritate the bladder
- Practicing pelvic floor exercises to strengthen muscles
- Managing stress through relaxation techniques like yoga or meditation
Physical Therapy
Physical therapy focused on the pelvic floor can be beneficial for men with chronic pelvic pain syndrome. Techniques such as myofascial release and biofeedback can help relieve muscle tension and improve symptoms.
Alternative Therapies
Some men find relief through alternative therapies such as acupuncture or herbal supplements. While scientific evidence supporting these treatments is limited, they may be worth exploring under the guidance of a healthcare provider.
Surgical Interventions
In rare cases where other treatments have failed, surgical procedures may be considered. These interventions aim to relieve pressure on the prostate or address structural abnormalities contributing to the condition.