A prolapsed disc, commonly referred to as a slipped disc, is a condition that affects the spine and can cause significant discomfort. While the term “slipped disc” is widely used, it is important to note that the disc itself does not actually slip out of place. Instead, the soft inner material of the disc protrudes through its outer layer, leading to potential compression of nearby nerves. This condition can result in pain, weakness, or numbness in various parts of the body, depending on the location of the affected disc. In this article, we will explore the causes, symptoms, and available treatments for this common spinal issue.

Understanding the Spine and Discs
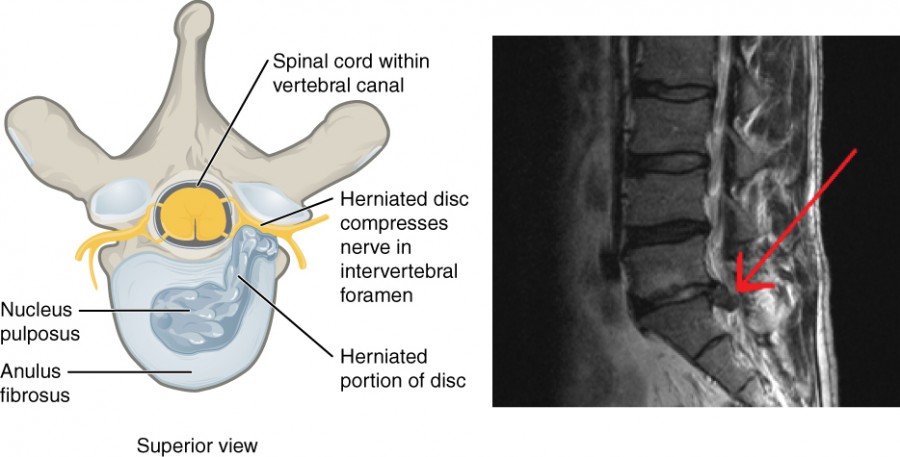
The spine is a complex structure made up of bones, muscles, ligaments, and discs. These components work together to provide support, flexibility, and protection for the spinal cord. The discs, which are located between each vertebra, act as cushions to absorb shock and prevent friction during movement. Each disc consists of two main parts: a tough outer layer called the annulus fibrosus and a soft, gel-like center known as the nucleus pulposus.
When a disc becomes damaged or weakened, the inner material may push through the outer layer. This condition is known as a prolapsed disc. Depending on the severity of the protrusion, it can press against nearby nerves, causing a range of symptoms.
Causes of a Prolapsed Disc
Several factors can contribute to the development of a prolapsed disc. Understanding these causes can help individuals take preventive measures to reduce their risk.
Age-Related Degeneration
As people age, the discs in the spine naturally lose water content and elasticity. This degeneration makes them more prone to injury or damage. Over time, the outer layer of the disc may weaken, increasing the likelihood of the inner material pushing through.
Injury or Trauma
Sudden trauma, such as a fall or car accident, can cause immediate damage to the discs. Even minor injuries that occur over time, such as repetitive lifting or twisting motions, can weaken the discs and lead to a prolapse.
Poor Posture
Maintaining poor posture for extended periods can place excessive strain on the spine and its supporting structures. Slouching, sitting for long hours, or lifting heavy objects incorrectly can increase the risk of disc damage.
Obesity
Excess body weight places additional pressure on the spine, particularly in the lower back. This added stress can accelerate disc degeneration and increase the likelihood of a prolapsed disc.
Genetic Factors
Some individuals may have a genetic predisposition to disc problems. If family members have experienced similar issues, there may be an increased risk of developing a prolapsed disc.
Symptoms of a Prolapsed Disc
The symptoms of a prolapsed disc can vary depending on the location of the affected disc and the extent of nerve compression. Some individuals may experience mild discomfort, while others may face severe pain or functional limitations.
Back Pain
One of the most common symptoms of a prolapsed disc is localized pain in the back. This pain may be sharp or dull and can worsen with movement or prolonged sitting.
Radiating Pain
If the prolapsed disc presses on a nerve, it can cause pain that radiates to other parts of the body. For example, a prolapsed disc in the lower back may lead to pain that travels down the leg, a condition known as sciatica.
Numbness and Tingling
Nerve compression can also result in sensations of numbness or tingling in the affected area. These symptoms often occur in the arms or legs, depending on the location of the disc problem.
Muscle Weakness
In some cases, a prolapsed disc can cause muscle weakness in the areas served by the affected nerve. This may make it difficult to perform everyday tasks, such as lifting objects or walking.
Bowel or Bladder Dysfunction
In rare cases, a prolapsed disc can lead to compression of the nerves responsible for controlling bowel or bladder function. This is considered a medical emergency and requires immediate attention.
Diagnosing a Prolapsed Disc
Proper diagnosis is essential for determining the most effective treatment plan. A healthcare provider will typically begin by conducting a thorough physical examination and reviewing the patient’s medical history. They may also order imaging tests to confirm the presence of a prolapsed disc.
Physical Examination
During the physical exam, the healthcare provider will assess the patient’s range of motion, reflexes, and muscle strength. They may also apply pressure to specific areas of the spine to identify the source of pain.
Imaging Tests
- Magnetic Resonance Imaging (MRI): This test provides detailed images of the spine and can clearly show the location and severity of a prolapsed disc.
- Computed Tomography (CT) Scan: A CT scan uses X-rays to create cross-sectional images of the spine. It can help identify bone abnormalities or disc herniation.
- X-Ray: While X-rays cannot directly show a prolapsed disc, they can help rule out other conditions, such as fractures or tumors.
Treatment Options for a Prolapsed Disc
Treatment for a prolapsed disc depends on the severity of symptoms and the impact on daily life. In many cases, conservative measures are sufficient to alleviate discomfort and promote healing. However, more severe cases may require advanced interventions.
Conservative Treatments
Rest and Activity Modification
Short-term rest can help reduce inflammation and allow the disc to heal. However, prolonged bed rest is generally discouraged, as it can lead to muscle weakness. Instead, individuals are encouraged to modify their activities and avoid movements that exacerbate symptoms.
Physical Therapy
Physical therapy plays a crucial role in managing a prolapsed disc. A therapist can design a personalized exercise program to strengthen the muscles supporting the spine, improve flexibility, and reduce pain.
Medications
Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help manage mild to moderate pain. In more severe cases, a healthcare provider may prescribe stronger medications, such as muscle relaxants or corticosteroids.
Heat and Ice Therapy
Applying heat or ice to the affected area can provide temporary relief from pain and inflammation. Heat helps relax tense muscles, while ice reduces swelling and numbs the area.
Advanced Treatments
Epidural Steroid Injections
For individuals experiencing persistent pain, epidural steroid injections may be recommended. These injections deliver anti-inflammatory medication directly to the affected area, providing targeted relief.
Minimally Invasive Procedures
In some cases, minimally invasive procedures, such as percutaneous discectomy or laser therapy, may be performed to remove or shrink the portion of the disc causing nerve compression.
Surgical Intervention
Surgery is typically reserved for cases where conservative treatments have failed or when there is significant nerve damage. Common surgical procedures include discectomy, laminectomy, or spinal fusion, depending on the specific needs of the patient.
Preventing a Prolapsed Disc
While not all cases of prolapsed discs can be prevented, certain lifestyle changes can reduce the risk of developing this condition.
Maintain a Healthy Weight
Excess weight places additional strain on the spine, so maintaining a healthy weight through diet and exercise can help protect the discs.
Practice Good Posture
Proper posture reduces stress on the spine and its supporting structures. Individuals should be mindful of their posture while sitting, standing, and lifting objects.
Exercise Regularly
Regular physical activity strengthens the muscles supporting the spine and improves overall flexibility. Low-impact exercises, such as swimming or yoga, are particularly beneficial.
Lift Objects Safely
When lifting heavy objects, individuals should bend at the knees and use their leg muscles rather than their back. This technique helps distribute the weight evenly and minimizes strain on the spine.
Quit Smoking
Smoking can impair blood flow to the discs, accelerating degeneration. Quitting smoking can improve overall spinal health and reduce the risk of disc problems.
Living with a Prolapsed Disc
Managing a prolapsed disc often requires a combination of medical treatment and lifestyle adjustments. By working closely with healthcare providers and adhering to recommended therapies, individuals can effectively manage their symptoms and maintain an active lifestyle.