Progressive Supranuclear Palsy, commonly abbreviated as PSP, is a rare and progressive neurological disorder that affects movement, balance, speech, vision, and cognition. It belongs to a group of conditions known as atypical parkinsonian disorders. Although the exact cause of this condition remains unknown, it is characterized by the gradual degeneration of brain cells, particularly in areas responsible for controlling movement and coordination. This article provides an in-depth look into the condition, its symptoms, diagnostic methods, and care strategies.
Understanding Progressive Supranuclear Palsy
Progressive Supranuclear Palsy is a complex neurodegenerative disease that primarily impacts older adults, typically beginning after the age of 60. It is often mistaken for Parkinson’s disease due to overlapping symptoms such as stiffness, slow movements, and balance problems. However, there are key differences that set it apart. Unlike Parkinson’s, this condition tends to progress more rapidly and includes unique symptoms like difficulty moving the eyes, especially looking downward.
The exact prevalence of this condition is not well-documented, but it is considered rare, affecting approximately five to six people per 100,000. The disease is caused by the abnormal accumulation of a protein called tau in the brain, which leads to the destruction of nerve cells. This buildup disrupts communication between neurons, ultimately leading to the characteristic symptoms of the condition.
Risk Factors
- Age: The risk increases significantly with age, particularly after 60 years.
- Genetics: While most cases occur sporadically, some individuals may have a family history of neurodegenerative diseases.
- Environmental Factors: Exposure to certain toxins or head injuries might contribute to the development of the condition, though research in this area is ongoing.
Symptoms of Progressive Supranuclear Palsy
The symptoms of this condition vary widely among individuals but generally worsen over time. Early signs can be subtle and easily overlooked, often leading to delayed diagnosis. Understanding these symptoms is crucial for early detection and management.
Motor Symptoms
One of the hallmark features of this condition is the difficulty in controlling eye movements, particularly when trying to look downward. This symptom often appears early in the disease and can make activities like reading or navigating stairs challenging. Other motor symptoms include:
- Balance Problems: Individuals may experience frequent falls, often backward, due to poor postural stability.
- Stiffness: Muscles become rigid, making movement slow and laborious.
- Slurred Speech: Speech may become slow, slurred, or monotone.
- Dysphagia: Difficulty swallowing can lead to choking or aspiration pneumonia.
Cognitive and Behavioral Changes
In addition to motor symptoms, individuals with this condition often experience cognitive decline and behavioral changes. These symptoms can include:
- Memory Problems: While memory loss is not as severe as in Alzheimer’s disease, individuals may struggle with planning, problem-solving, and multitasking.
- Mood Changes: Depression, apathy, and irritability are common emotional symptoms.
- Impulsivity: Some individuals may exhibit impulsive behaviors, such as overeating or inappropriate social conduct.
Other Symptoms
As the disease progresses, additional symptoms may emerge, including:
- Sleep Disturbances: Insomnia, restless leg syndrome, or REM sleep behavior disorder can occur.
- Bladder Dysfunction: Urinary urgency or incontinence may develop.
- Fatigue: Persistent tiredness can significantly impact quality of life.
Diagnosis of Progressive Supranuclear Palsy
Diagnosing this condition can be challenging due to its similarity to other neurodegenerative disorders. There is no single test to confirm the presence of the disease, so healthcare providers rely on a combination of clinical evaluations, imaging studies, and ruling out other conditions.
Clinical Evaluation
A thorough medical history and neurological examination are essential for identifying potential symptoms. During the evaluation, doctors will assess:
- Gait and balance
- Eye movements
- Muscle tone and reflexes
- Cognitive function
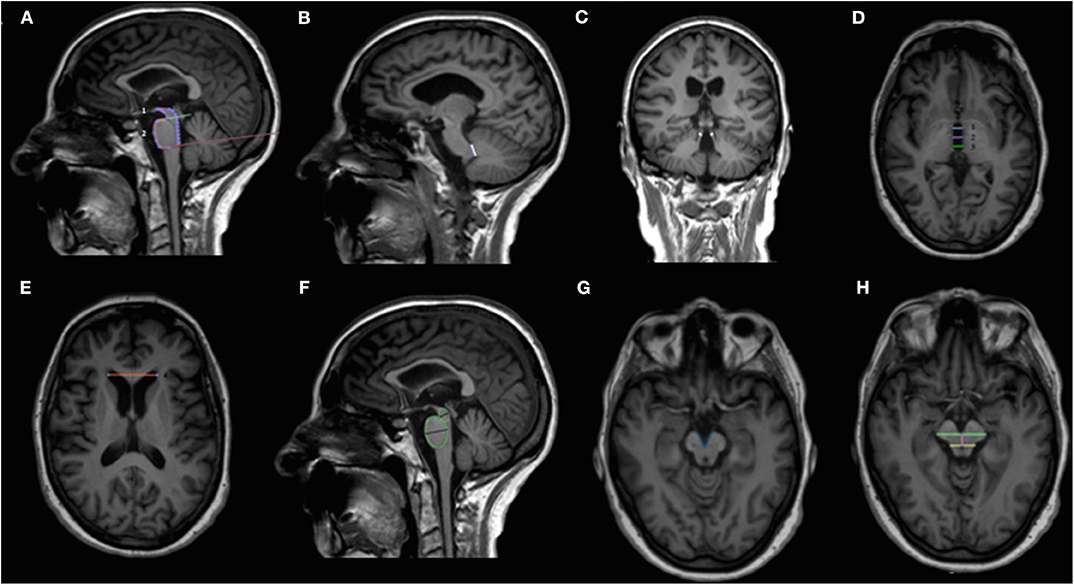
Imaging Studies
Brain imaging techniques such as magnetic resonance imaging (MRI) or positron emission tomography (PET) scans may be used to detect structural changes in the brain. In individuals with this condition, imaging often reveals shrinkage in specific brain regions, particularly those involved in movement control.
Ruling Out Other Conditions
Because the symptoms overlap with other disorders, such as Parkinson’s disease or multiple system atrophy, doctors may perform additional tests to exclude these possibilities. Blood tests, lumbar punctures, or specialized imaging studies may be necessary to confirm the diagnosis.
Care and Management Strategies
While there is currently no cure for this condition, several treatment options and supportive care measures can help manage symptoms and improve quality of life. A multidisciplinary approach involving healthcare professionals from various fields is often recommended.
Medications
Although medications cannot halt the progression of the disease, they can alleviate certain symptoms:
- Parkinson’s Medications: Drugs like levodopa may provide limited relief for stiffness and slowness of movement, though they are often less effective than in Parkinson’s disease.
- Antidepressants: These can help manage mood changes and depression.
- Botox Injections: Botulinum toxin may be used to treat excessive drooling or dystonia (involuntary muscle contractions).
Physical and Occupational Therapy
Therapies play a vital role in maintaining mobility and independence:
- Physical Therapy: Exercises designed to improve strength, flexibility, and balance can reduce the risk of falls.
- Occupational Therapy: Adaptive techniques and tools can help individuals perform daily tasks more easily.
- Speech Therapy: Techniques to improve speech clarity and swallowing safety are beneficial.
Nutritional Support
Difficulty swallowing can lead to malnutrition or dehydration, so dietary adjustments are often necessary:
- Soft Foods: Pureed or soft foods can reduce the risk of choking.
- Hydration: Ensuring adequate fluid intake is critical to prevent complications.
- Feeding Tubes: In advanced cases, a feeding tube may be required to ensure proper nutrition.
Emotional and Psychological Support
Coping with a progressive illness can be emotionally taxing for both patients and their families. Counseling, support groups, and educational resources can provide valuable assistance:
- Individual Counseling: Helps individuals process emotions and develop coping strategies.
- Support Groups: Connecting with others facing similar challenges can reduce feelings of isolation.
- Family Education: Teaching caregivers about the disease and its progression fosters understanding and preparedness.
Palliative and Hospice Care
In the later stages of the disease, palliative care focuses on comfort and quality of life. Hospice services may be introduced to provide comprehensive end-of-life care, ensuring dignity and respect for the individual.
Research and Future Directions
Ongoing research aims to better understand the underlying causes of this condition and develop targeted therapies. Clinical trials are exploring new medications, gene therapies, and interventions to slow disease progression. Advances in imaging technology and biomarker identification hold promise for earlier and more accurate diagnoses.
Collaboration between researchers, clinicians, and advocacy organizations is essential to accelerate progress in this field. Increased awareness and funding can help address the unmet needs of individuals living with this challenging condition.





