Primary Biliary Cholangitis, commonly abbreviated as PBC, is a chronic autoimmune disease that affects the bile ducts in the liver. This condition leads to inflammation and gradual destruction of these ducts, impairing the liver’s ability to function properly. Over time, this damage can result in serious complications, including cirrhosis and liver failure. Understanding Primary Biliary Cholangitis is crucial for early diagnosis and effective management of the disease.
What is Primary Biliary Cholangitis?
Primary Biliary Cholangitis is a rare but progressive disease that primarily targets the small bile ducts within the liver. The bile ducts are responsible for transporting bile, a digestive fluid produced by the liver, to the gallbladder and intestines. When these ducts are damaged or destroyed, bile accumulates in the liver, leading to inflammation and scarring. This process ultimately compromises liver function and can lead to severe health issues if left untreated.
How Common is Primary Biliary Cholangitis?
- Primary Biliary Cholangitis is considered a rare disease, affecting approximately 1 in 1,000 women over the age of 40.
- It is more prevalent in women than men, with a female-to-male ratio of about 9:1.
- The condition is most commonly diagnosed in individuals between the ages of 30 and 60.
Causes of Primary Biliary Cholangitis
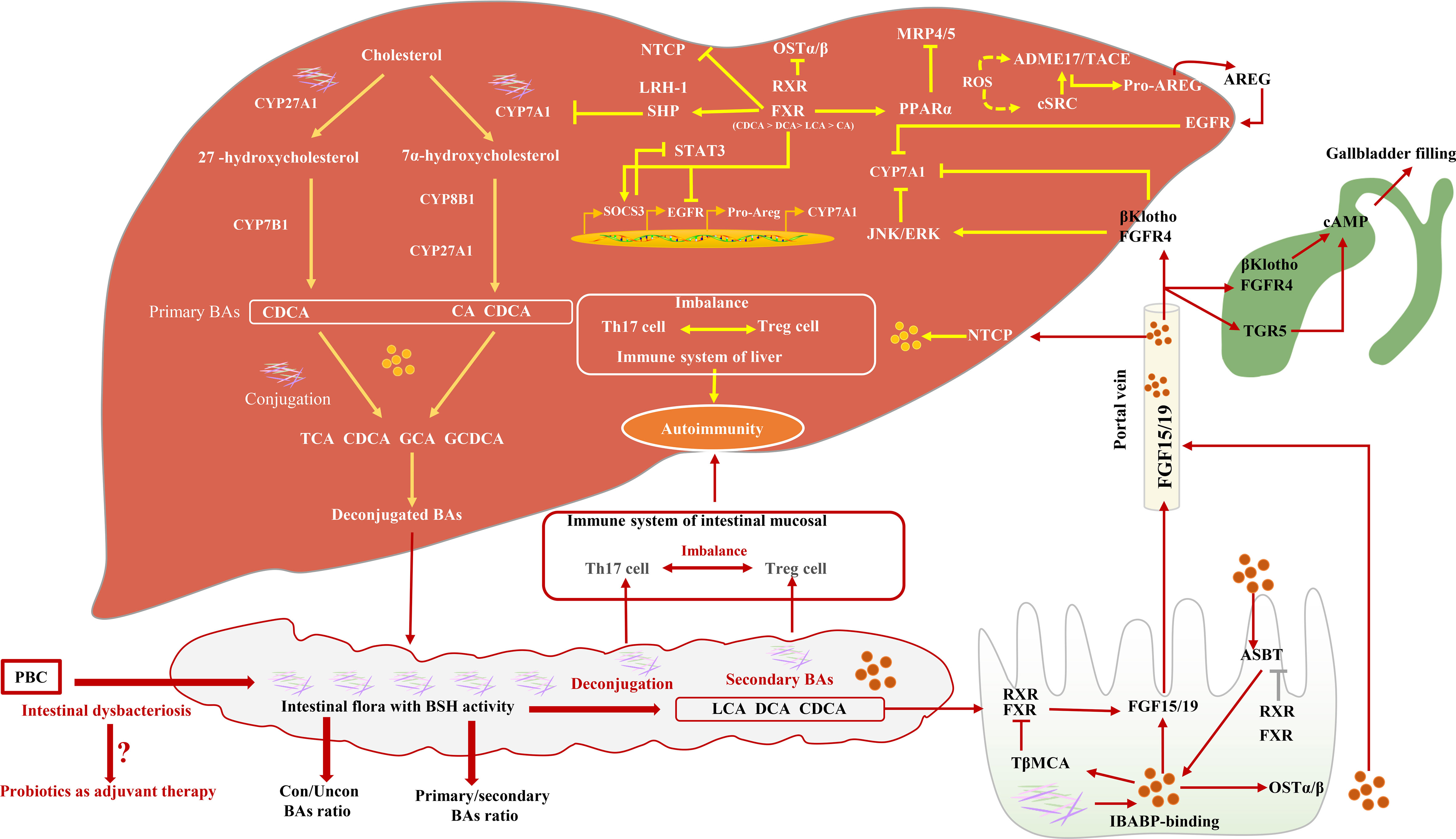
The exact cause of Primary Biliary Cholangitis remains unknown, but research suggests that it is an autoimmune disorder. In autoimmune diseases, the body’s immune system mistakenly attacks its own healthy tissues. In the case of this condition, the immune system targets the bile ducts, leading to their inflammation and eventual destruction.
Potential Contributing Factors
While the precise triggers are unclear, several factors may contribute to the development of this disease:
- Genetics: A family history of autoimmune diseases increases the risk of developing Primary Biliary Cholangitis. Certain genetic markers have been identified in individuals with the condition.
- Environmental Triggers: Exposure to toxins, infections, or other environmental factors may play a role in triggering the disease in genetically predisposed individuals.
- Hormonal Influences: The higher prevalence of this condition in women suggests that hormones may influence its development.
Symptoms of Primary Biliary Cholangitis
In its early stages, Primary Biliary Cholangitis often does not cause noticeable symptoms. Many individuals are diagnosed during routine blood tests that reveal abnormal liver function. As the disease progresses, however, symptoms may begin to appear. These symptoms can vary in severity and may include:
Common Symptoms
- Fatigue: Persistent tiredness is one of the most frequently reported symptoms and can significantly impact daily life.
- Itching: Known as pruritus, this symptom is caused by the buildup of bile salts in the skin and can range from mild to severe.
- Dry Eyes and Mouth: Many individuals experience dryness in the eyes and mouth, which is often associated with an overlapping condition called Sjögren’s syndrome.
Advanced Symptoms
As the disease progresses and liver damage worsens, additional symptoms may develop:
- Jaundice: Yellowing of the skin and eyes occurs due to elevated levels of bilirubin in the blood.
- Swelling: Fluid retention in the abdomen (ascites) or legs (edema) may occur as liver function declines.
- Bone Pain and Fractures: Reduced absorption of vitamins and minerals can weaken bones, increasing the risk of fractures.
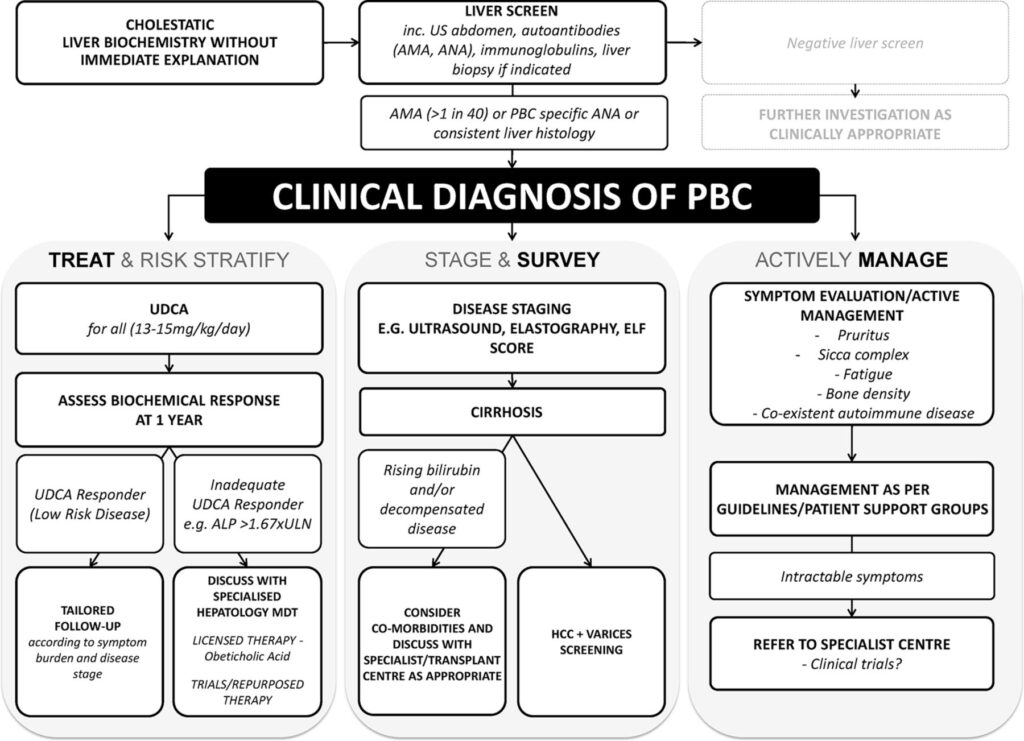
Diagnosis of Primary Biliary Cholangitis
Diagnosing Primary Biliary Cholangitis typically involves a combination of medical history evaluation, physical examination, and diagnostic tests. Early detection is essential for managing the disease effectively and preventing complications.
Diagnostic Tests
- Blood Tests: Elevated levels of alkaline phosphatase and specific antibodies, such as antimitochondrial antibodies, are key indicators of the condition.
- Imaging Studies: Ultrasound or MRI scans may be used to assess the structure and function of the liver and bile ducts.
- Liver Biopsy: In some cases, a small sample of liver tissue is taken for analysis to confirm the diagnosis and assess the extent of liver damage.
Treatment Options for Primary Biliary Cholangitis
While there is no cure for Primary Biliary Cholangitis, treatment focuses on slowing disease progression, managing symptoms, and preventing complications. Early intervention can significantly improve outcomes and quality of life for affected individuals.
Medications
- Ursodeoxycholic Acid: This medication helps improve bile flow and slow liver damage. It is often prescribed as a first-line treatment.
- Obeticholic Acid: Used in combination with or as an alternative to ursodeoxycholic acid, this drug reduces inflammation and fibrosis in the liver.
- Symptom Management: Medications may be prescribed to alleviate itching, fatigue, and other symptoms associated with the disease.
Lifestyle Modifications
In addition to medications, lifestyle changes can play a crucial role in managing the condition:
- Dietary Adjustments: A balanced diet low in fat and sodium can help reduce symptoms and support liver health.
- Vitamin Supplements: Individuals with this condition may require supplements to address deficiencies in fat-soluble vitamins (A, D, E, and K).
- Regular Exercise: Physical activity can help combat fatigue and improve overall well-being.
Complications of Primary Biliary Cholangitis
If left untreated or poorly managed, Primary Biliary Cholangitis can lead to serious complications. These complications arise as a result of progressive liver damage and impaired function.
Potential Complications
- Cirrhosis: Scarring of the liver tissue can impair its ability to function properly, leading to liver failure.
- Liver Cancer: Individuals with advanced liver disease are at an increased risk of developing hepatocellular carcinoma.
- Osteoporosis: Bone density loss is common in individuals with this condition, increasing the risk of fractures.
- Portal Hypertension: Increased pressure in the portal vein can cause complications such as varices and gastrointestinal bleeding.
Living with Primary Biliary Cholangitis
Managing Primary Biliary Cholangitis requires a comprehensive approach that addresses both physical and emotional well-being. Support from healthcare providers, family, and peers can make a significant difference in coping with the challenges of the disease.
Emotional and Mental Health
Living with a chronic illness can take a toll on mental health. Individuals with this condition may experience anxiety, depression, or feelings of isolation. Seeking professional counseling or joining support groups can provide valuable emotional support and practical advice.
Regular Monitoring
Regular follow-up appointments with healthcare providers are essential for monitoring disease progression and adjusting treatment plans as needed. Routine blood tests, imaging studies, and other assessments help ensure that any complications are detected and addressed promptly.
Future Directions in Research and Treatment
Ongoing research into Primary Biliary Cholangitis aims to uncover new insights into its causes, improve diagnostic methods, and develop more effective treatments. Advances in understanding the genetic and immunological mechanisms underlying the disease hold promise for targeted therapies that could revolutionize care for affected individuals.
Emerging Therapies
- Biologic Agents: Researchers are exploring the use of biologic drugs to modulate the immune response and reduce inflammation in the liver.
- Stem Cell Therapy: Experimental treatments involving stem cells aim to regenerate damaged liver tissue and restore function.
- Gene Therapy: Efforts are underway to identify genetic targets for intervention, potentially offering personalized treatment options.