Prader-Willi Syndrome, often abbreviated as PWS, is a rare genetic disorder that affects multiple systems in the body. It is characterized by a range of physical, cognitive, and behavioral symptoms that require lifelong management. This article explores the underlying causes of this condition, its hallmark symptoms, and strategies for effective management.
Understanding the Causes
The origins of Prader-Willi Syndrome lie in a genetic anomaly involving chromosome 15. Specifically, it occurs when certain genes on the father’s chromosome 15 are missing or not functioning properly. To better understand this, let us delve into the mechanisms behind the condition.
Genetic Mechanisms
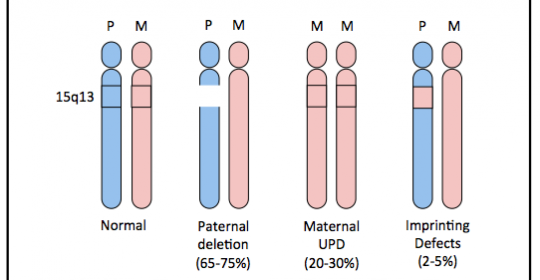
- Paternal Deletion: In approximately 70 percent of cases, a segment of the father’s chromosome 15 is missing. This deletion prevents the expression of critical genes responsible for normal development and function.
- Maternal Uniparental Disomy: In about 25 percent of cases, the individual inherits both copies of chromosome 15 from the mother instead of one from each parent. This leads to an imbalance in gene expression.
- Imprinting Center Defects: In rare instances, mutations occur in the imprinting center of chromosome 15, disrupting the regulation of gene activity. This defect can originate from either parent.
Risk Factors and Genetic Counseling
Prader-Willi Syndrome is not typically inherited in a straightforward manner, as most cases arise spontaneously due to random genetic errors. However, families with a history of the condition may benefit from genetic counseling to assess risks and explore reproductive options.
Recognizing the Symptoms
The symptoms of this syndrome vary depending on the individual’s age and developmental stage. Early recognition is crucial for timely intervention and improved outcomes. Below, we outline the key symptoms observed during different life stages.
Symptoms in Infancy
- Hypotonia: Newborns often exhibit poor muscle tone, making them appear “floppy.” This can lead to difficulties with feeding and gaining weight.
- Feeding Difficulties: Weak sucking reflexes and an inability to feed effectively are common, often requiring specialized feeding techniques or medical support.
- Delayed Development: Milestones such as rolling over, sitting up, and walking may be significantly delayed compared to typical infants.
Symptoms in Childhood
- Hyperphagia: As children grow older, they develop an insatiable appetite, which can lead to excessive weight gain if not carefully managed.
- Obesity Risk: Without intervention, the combination of hyperphagia and reduced energy expenditure places individuals at high risk for obesity-related complications.
- Cognitive Challenges: Most children experience mild to moderate intellectual disabilities, impacting learning and social interactions.
- Behavioral Issues: Temper tantrums, stubbornness, and obsessive-compulsive tendencies are frequently observed.
Symptoms in Adolescence and Adulthood
- Hormonal Imbalances: Many individuals experience growth hormone deficiencies, leading to short stature and delayed puberty.
- Sleep Disorders: Conditions such as sleep apnea are prevalent due to obesity and structural abnormalities in the airway.
- Skin Picking: A compulsive habit of picking at the skin, particularly around the hands and arms, is common and may result in infections or scarring.
Managing the Condition
While there is no cure for this syndrome, a multidisciplinary approach can significantly improve quality of life. Effective management involves addressing physical, nutritional, behavioral, and psychological needs through tailored interventions.
Nutritional Management
One of the most critical aspects of care is managing food intake to prevent obesity and its associated health risks. Strategies include:
- Controlled Access to Food: Keeping food out of reach and establishing strict meal schedules helps regulate consumption.
- Balanced Diet: A dietitian can design a nutrient-dense, low-calorie meal plan to meet the individual’s needs without promoting weight gain.
- Regular Monitoring: Frequent check-ins with healthcare providers ensure that weight and nutritional status remain within healthy ranges.
Growth Hormone Therapy
Growth hormone treatment is often recommended to address short stature and improve muscle tone. Benefits of this therapy include:
- Increased Height: Children receiving growth hormone tend to achieve greater height than those who do not.
- Improved Muscle Mass: Enhanced muscle strength supports mobility and reduces fatigue.
- Better Metabolism: Growth hormone can help optimize energy expenditure and reduce fat accumulation.
Behavioral and Psychological Support
Addressing behavioral challenges requires patience and consistency. Interventions may include:
- Behavioral Therapy: Techniques such as positive reinforcement and structured routines can mitigate problematic behaviors.
- Mental Health Services: Counseling and psychiatric support are essential for managing anxiety, depression, or other mental health concerns.
- Social Skills Training: Teaching communication and interpersonal skills fosters independence and enhances relationships.
Medical Monitoring and Interventions
Regular medical evaluations are necessary to detect and manage complications early. Key areas of focus include:
- Sleep Studies: Diagnosing and treating sleep disorders like sleep apnea improves overall well-being.
- Orthopedic Care: Addressing issues such as scoliosis or joint problems ensures proper physical development.
- Hormonal Assessments: Evaluating thyroid function and sex hormone levels guides appropriate treatments.
Family and Caregiver Education
Families play a vital role in managing the condition. Educating caregivers about the syndrome’s complexities empowers them to provide optimal support. Resources such as workshops, online forums, and advocacy groups offer valuable guidance and community connections.
Looking Ahead
Ongoing research continues to shed light on the genetic and physiological underpinnings of this syndrome. Advances in gene therapy and personalized medicine hold promise for more targeted treatments in the future. Meanwhile, raising awareness and fostering understanding among healthcare professionals and the general public remains essential for improving outcomes for affected individuals.