Postherpetic neuralgia, often abbreviated as PHN, is a condition that arises after an individual has experienced shingles. It is characterized by persistent nerve pain that continues long after the rash and blisters associated with shingles have healed. This condition can significantly impact the quality of life for those affected, making it essential to understand its causes, symptoms, diagnosis, and treatment options.
What Causes Postherpetic Neuralgia?
The root cause of postherpetic neuralgia lies in the damage inflicted on nerve fibers during a shingles outbreak. To fully comprehend this, it is important to first understand the connection between shingles and the varicella-zoster virus.
The Role of the Varicella-Zoster Virus
The varicella-zoster virus is responsible for two distinct conditions: chickenpox and shingles. When a person contracts chickenpox, the virus does not leave the body entirely after recovery. Instead, it remains dormant in the nervous system, specifically within the nerve tissue near the spinal cord and brain. Years or even decades later, the virus can reactivate, leading to shingles.
How Nerve Damage Leads to Persistent Pain
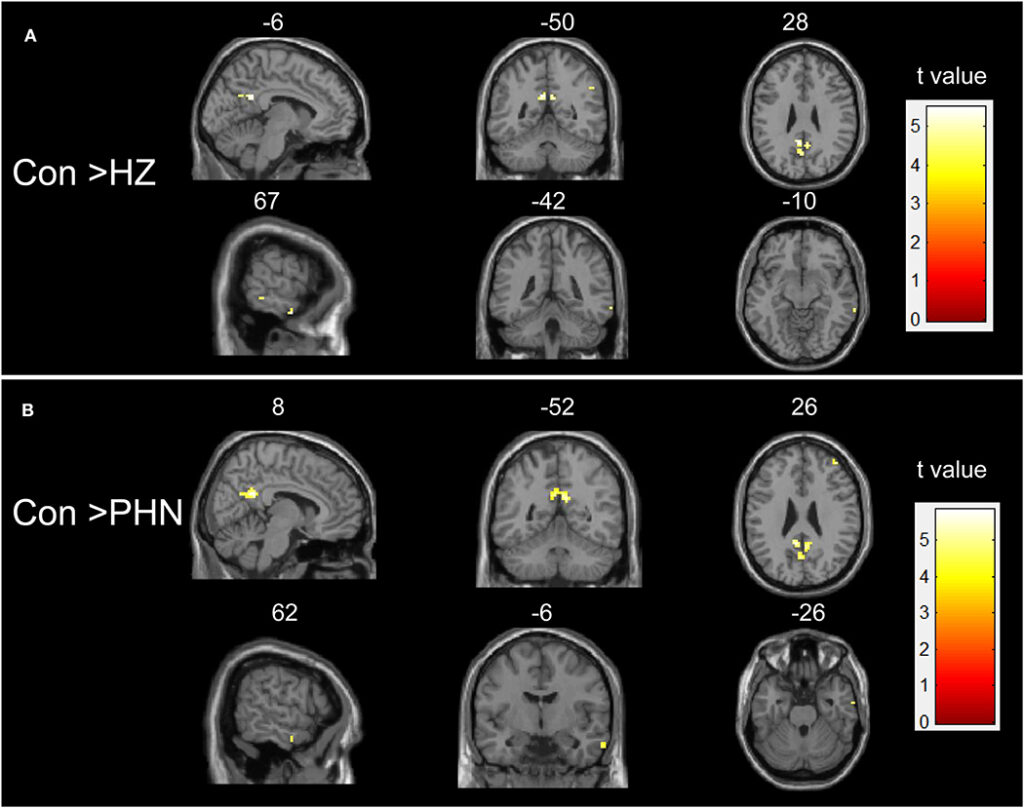
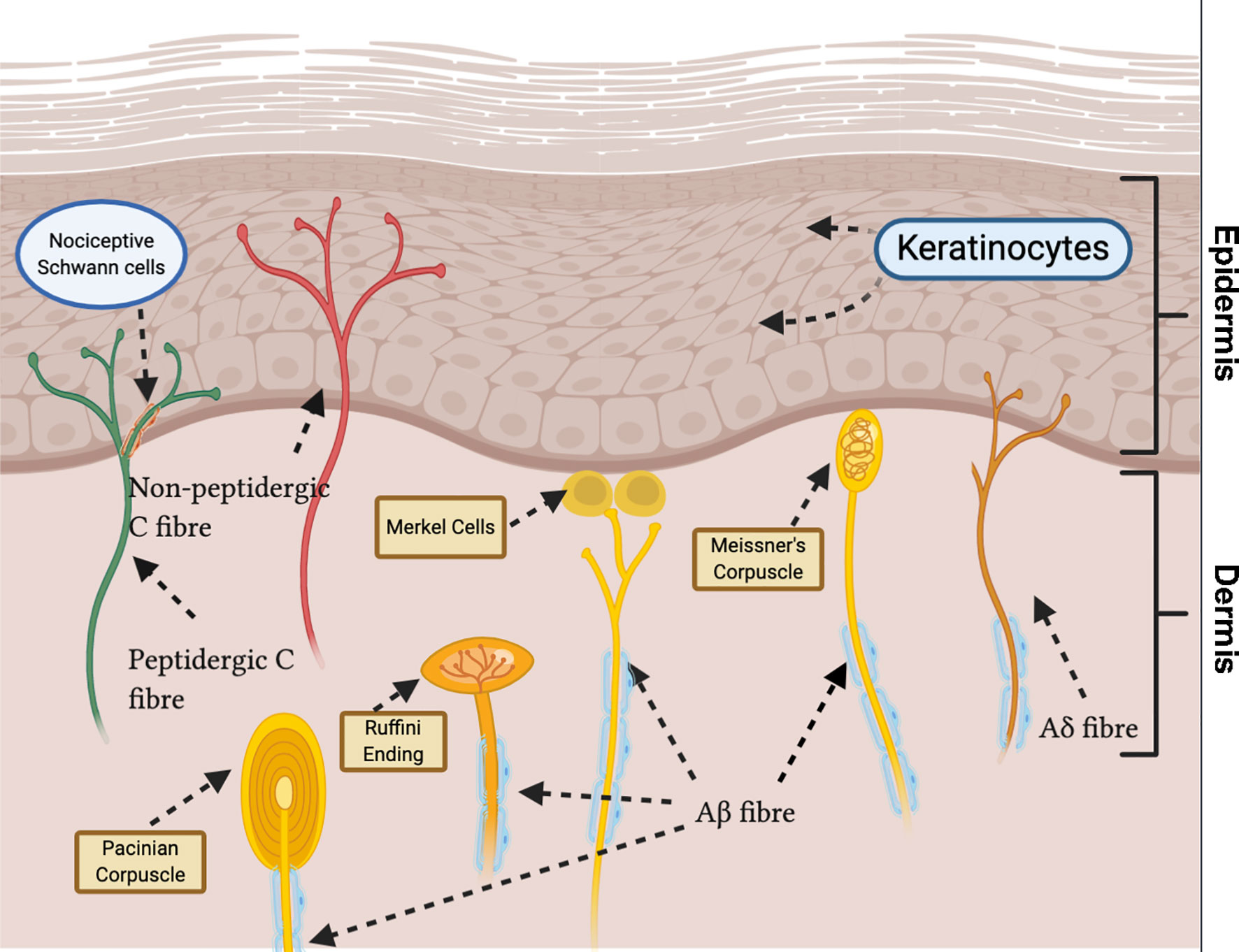
During a shingles outbreak, the reactivated virus travels along nerve pathways to the skin, causing a painful rash. In some cases, the inflammation and damage caused by the virus affect the nerve fibers, disrupting their ability to send messages from the skin to the brain. As a result, the affected nerves may send exaggerated or incorrect pain signals, even after the shingles rash has healed. This ongoing nerve pain is what defines postherpetic neuralgia.
Symptoms of Postherpetic Neuralgia
The symptoms of postherpetic neuralgia are primarily centered around pain, but they can vary in intensity and duration depending on the individual. Below are the most common manifestations of this condition:
- Burning Sensation: Many individuals describe the pain as a constant burning feeling in the area where the shingles rash occurred.
- Sharp or Jabbing Pain: Sudden, intense bursts of pain may occur intermittently, adding to the discomfort.
- Sensitivity to Touch: Even light pressure, such as from clothing or a gentle touch, can trigger severe pain in the affected area.
- Numbness or Tingling: Some people experience a loss of sensation or a tingling sensation in the region affected by the nerve damage.
- Itching: Persistent itching may accompany the pain, further complicating the condition.
Duration of Symptoms
The duration of postherpetic neuralgia varies widely. For some individuals, the pain subsides within weeks or months. However, for others, it can persist for years, becoming a chronic condition. The likelihood of developing prolonged symptoms increases with age, particularly in individuals over the age of sixty.
Risk Factors for Developing Postherpetic Neuralgia
While anyone who has had shingles is at risk of developing this condition, certain factors increase the likelihood of experiencing prolonged nerve pain:
- Age: Older adults, especially those over sixty, are more susceptible to postherpetic neuralgia due to the natural decline in nerve function that occurs with aging.
- Severity of Shingles: Individuals who experience severe pain or extensive rashes during their shingles outbreak are more likely to develop this condition.
- Existing Health Conditions: People with conditions such as diabetes or weakened immune systems are at a higher risk because these factors can exacerbate nerve damage.
- Delayed Treatment for Shingles: Failing to seek prompt medical attention for shingles can increase the risk of complications, including postherpetic neuralgia.
Diagnosing Postherpetic Neuralgia
Diagnosing this condition typically involves a thorough evaluation of the patient’s medical history and symptoms. Since there is no specific test to confirm postherpetic neuralgia, healthcare providers rely on the following steps:
Medical History and Physical Examination
A doctor will begin by asking about the patient’s history of shingles, including when the outbreak occurred and the severity of the symptoms. They will also conduct a physical examination to assess the affected area for signs of lingering pain, sensitivity, or other abnormalities.
Ruling Out Other Conditions
Because the symptoms of postherpetic neuralgia can overlap with other conditions, such as fibromyalgia or diabetic neuropathy, additional tests may be necessary. These could include blood tests, imaging studies, or nerve conduction studies to rule out alternative causes of the pain.
Treatment Options for Postherpetic Neuralgia
While there is no cure for postherpetic neuralgia, several treatment approaches can help manage the pain and improve the patient’s quality of life. These treatments often involve a combination of medications, therapies, and lifestyle adjustments.
Medications
Various medications are commonly prescribed to alleviate the symptoms of postherpetic neuralgia:
- Pain Relievers: Over-the-counter pain relievers, such as acetaminophen or ibuprofen, may provide mild relief. For more severe pain, prescription medications like opioids may be considered, though they carry a risk of dependency.
- Anticonvulsants: Medications originally developed to treat seizures, such as gabapentin and pregabalin, are effective in reducing nerve-related pain.
- Antidepressants: Certain antidepressants, such as tricyclic antidepressants, can help regulate pain signals in the nervous system.
- Topical Treatments: Lidocaine patches or capsaicin cream applied directly to the affected area can provide localized relief.
Therapies
In addition to medications, various therapies can complement the treatment plan:
- Physical Therapy: Exercises designed to improve strength and flexibility can help reduce pain and prevent muscle weakness in the affected area.
- Nerve Blocks: Injections of anesthetic or steroid medications near the affected nerves can temporarily block pain signals.
- Transcutaneous Electrical Nerve Stimulation (TENS): This non-invasive therapy uses low-voltage electrical currents to relieve pain by stimulating the nerves.
Lifestyle Adjustments
Making certain lifestyle changes can also contribute to managing the symptoms of postherpetic neuralgia:
- Stress Management: Techniques such as meditation, deep breathing exercises, or yoga can help reduce stress, which may alleviate pain.
- Dietary Changes: Consuming a balanced diet rich in anti-inflammatory foods, such as fruits, vegetables, and omega-3 fatty acids, may support nerve health.
- Protecting the Skin: Avoiding tight clothing or anything that irritates the affected area can minimize discomfort.
Preventing Postherpetic Neuralgia
While not all cases of postherpetic neuralgia can be prevented, certain measures can reduce the risk of developing this condition:
Vaccination Against Shingles
One of the most effective ways to prevent postherpetic neuralgia is to avoid getting shingles in the first place. The shingles vaccine is recommended for adults over the age of fifty and has been shown to significantly reduce the risk of developing shingles and its complications.
Prompt Treatment for Shingles
If shingles do occur, seeking medical attention early can help minimize nerve damage. Antiviral medications, when started within seventy-two hours of the onset of the rash, can reduce the severity and duration of the outbreak, thereby lowering the risk of postherpetic neuralgia.
Maintaining a Healthy Lifestyle
Boosting the immune system through regular exercise, adequate sleep, and a nutritious diet can also play a role in preventing shingles and its complications. Additionally, managing chronic conditions like diabetes can help protect nerve health.
Living with Postherpetic Neuralgia
For those living with this condition, finding effective ways to cope with the pain is crucial. Support groups, counseling, and open communication with healthcare providers can provide valuable resources and guidance. Experimenting with different treatment combinations under medical supervision may also lead to better outcomes.