Pneumonitis, often abbreviated as PN, is a condition characterized by inflammation of the lung tissue. This inflammation can result from various factors, including exposure to harmful substances, infections, or underlying medical conditions. Unlike pneumonia, which is caused by an infection, pneumonitis is primarily triggered by non-infectious agents. Understanding its causes, symptoms, diagnostic methods, and treatment options is crucial for managing this condition effectively.
What is Pneumonitis?
Pneumonitis refers to the inflammation of the air sacs in the lungs, known as alveoli. When these air sacs become inflamed, they may fill with fluid or other substances, making it difficult for oxygen to pass into the bloodstream. This condition can lead to breathing difficulties and other complications if left untreated. While pneumonitis shares some similarities with pneumonia, the two are distinct conditions with different underlying causes.
Common Types of Pneumonitis
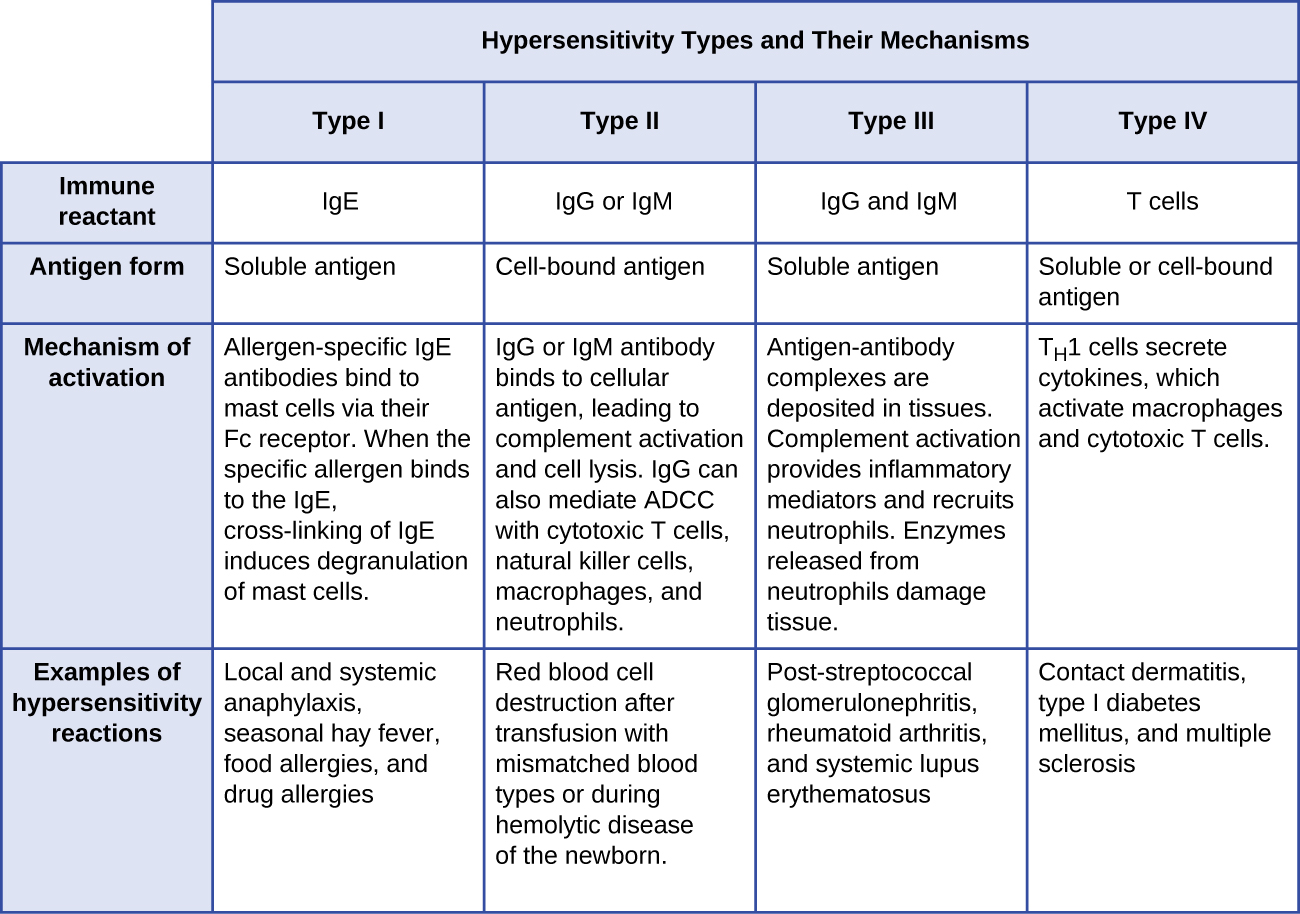
- Hypersensitivity pneumonitis: Caused by an allergic reaction to inhaled substances.
- Radiation pneumonitis: Occurs as a side effect of radiation therapy for cancer.
- Chemical pneumonitis: Triggered by inhaling toxic chemicals or fumes.
- Aspiration pneumonitis: Results from inhaling food, liquid, or vomit into the lungs.
Causes of Pneumonitis
The causes of pneumonitis vary widely and depend on the type of exposure or underlying health condition. Below are some of the most common causes of this condition:
Inhalation of Harmful Substances
One of the primary causes of pneumonitis is the inhalation of harmful substances. These substances can irritate the lungs and trigger an inflammatory response. Common examples include:
- Mold spores
- Bird droppings or feathers
- Dust from farming or construction work
- Chemical fumes from industrial settings
Individuals who work in environments where they are frequently exposed to these substances are at a higher risk of developing pneumonitis.
Radiation Therapy
Radiation therapy is a common treatment for certain types of cancer, particularly those affecting the chest area. However, this treatment can sometimes cause inflammation in the lungs, leading to radiation pneumonitis. The severity of this condition depends on the dose of radiation and the area of the lungs exposed.
Medications
Certain medications can also cause pneumonitis as a side effect. These include chemotherapy drugs, antibiotics, and heart medications. In some cases, the immune system may react adversely to these medications, resulting in inflammation of the lung tissue.
Aspiration
Aspiration occurs when foreign materials, such as food, liquid, or stomach contents, enter the lungs. This can happen due to swallowing difficulties, vomiting, or loss of consciousness. Aspiration pneumonitis is more common in individuals with neurological disorders or those under the influence of alcohol or sedatives.
Symptoms of Pneumonitis
The symptoms of pneumonitis can vary depending on the severity of the condition and the underlying cause. Some individuals may experience mild symptoms, while others may develop more severe complications. Common symptoms include:
Early Symptoms
- Shortness of breath, especially during physical activity
- Dry cough
- Fatigue
- Fever
These early symptoms may be mistaken for other respiratory conditions, such as asthma or bronchitis. As a result, pneumonitis is often underdiagnosed in its initial stages.
Advanced Symptoms
- Difficulty breathing even at rest
- Unexplained weight loss
- Clubbing of fingers or toes (a sign of chronic oxygen deprivation)
- Chest pain or tightness
If left untreated, pneumonitis can progress to chronic lung disease, such as pulmonary fibrosis, where scar tissue forms in the lungs, further impairing their function.
Diagnosis of Pneumonitis
Diagnosing pneumonitis can be challenging because its symptoms overlap with those of other respiratory conditions. A thorough evaluation is necessary to identify the underlying cause and determine the appropriate treatment. The diagnostic process typically involves the following steps:
Medical History and Physical Examination
A healthcare provider will begin by taking a detailed medical history, including information about occupational exposures, medications, and any recent illnesses. They will also perform a physical examination to check for signs of respiratory distress, such as wheezing or crackling sounds in the lungs.
Imaging Tests
Imaging tests are essential for visualizing the lungs and identifying areas of inflammation or damage. Common imaging techniques include:
- Chest X-ray: Provides a basic view of the lungs and can reveal abnormalities.
- Computed tomography (CT) scan: Offers a more detailed image of the lung tissue and can help identify specific patterns of inflammation.
Lung Function Tests
Lung function tests measure how well the lungs are working. These tests assess parameters such as lung capacity, airflow, and gas exchange. A decline in lung function may indicate the presence of pneumonitis.
Bronchoscopy
In some cases, a bronchoscopy may be performed to examine the airways and collect samples of lung tissue or fluid. This procedure involves inserting a thin, flexible tube with a camera into the lungs through the nose or mouth.
Blood Tests
Blood tests can help identify markers of inflammation or autoimmune diseases that may contribute to pneumonitis. They can also rule out infections as the cause of symptoms.
Treatment of Pneumonitis
The treatment of pneumonitis focuses on addressing the underlying cause, reducing inflammation, and preventing further damage to the lungs. The specific approach depends on the type and severity of the condition.
Identifying and Avoiding Triggers
For individuals with hypersensitivity pneumonitis, the first step in treatment is identifying and avoiding the substance causing the allergic reaction. This may involve making changes to the home or work environment, such as improving ventilation or using protective equipment.
Medications
Medications play a key role in managing pneumonitis. Commonly prescribed treatments include:
- Corticosteroids: These anti-inflammatory drugs help reduce swelling in the lungs and alleviate symptoms. Prednisone is a commonly used corticosteroid.
- Immunosuppressants: In cases where the immune system is overactive, medications that suppress immune activity may be prescribed.
Oxygen Therapy
For individuals with severe breathing difficulties, supplemental oxygen may be necessary to ensure adequate oxygen levels in the blood. Oxygen therapy can be administered through a mask or nasal cannula.
Lifestyle Changes
Making lifestyle changes can also help manage pneumonitis and improve overall lung health. These changes may include:
- Quitting smoking
- Engaging in regular, moderate exercise to strengthen the respiratory muscles
- Maintaining a healthy diet to support immune function
Treatment for Underlying Conditions
If pneumonitis is caused by an underlying medical condition, such as an autoimmune disorder, treating that condition is essential. This may involve a combination of medications, therapies, and lifestyle modifications.
Preventing Pneumonitis
While not all cases of pneumonitis can be prevented, there are steps individuals can take to reduce their risk. These include:
- Using protective gear, such as masks, when working in environments with airborne irritants
- Ensuring proper ventilation in homes and workplaces
- Avoiding exposure to mold, dust, and other allergens
- Following safety guidelines during radiation therapy or when taking medications known to cause lung inflammation
Regular check-ups with a healthcare provider can also help detect early signs of pneumonitis and prevent complications.