Pleural empyema, often abbreviated as PE, is a serious medical condition characterized by the accumulation of pus in the pleural space, which is the area between the lungs and the chest wall. This condition can lead to significant complications if not treated promptly. In this article, we will explore the causes, symptoms, diagnostic methods, and treatment options for pleural empyema in detail.

Understanding Pleural Empyema
The pleural space normally contains a small amount of fluid that helps the lungs move smoothly during breathing. However, when an infection occurs in this space, it can result in the buildup of pus, leading to pleural empyema. The presence of pus indicates an active infection, often caused by bacteria, and requires immediate medical attention.
Causes of Pleural Empyema
Pleural empyema can occur due to various reasons, with infections being the most common cause. Below are some of the primary factors that contribute to the development of this condition:
- Bacterial Pneumonia: The most frequent cause of pleural empyema is bacterial pneumonia. When bacteria from the lungs spread to the pleural space, they can trigger an infection that leads to pus formation.
- Lung Abscess: A lung abscess is a localized collection of pus within the lung tissue. If the abscess ruptures, it can release infectious material into the pleural space, causing empyema.
- Trauma or Surgery: Chest injuries or surgical procedures involving the lungs or chest cavity can introduce bacteria into the pleural space, increasing the risk of infection.
- Bloodstream Infections: In rare cases, bacteria from other parts of the body can travel through the bloodstream and infect the pleural space.
- Weakened Immune System: Individuals with weakened immune systems, such as those with diabetes, cancer, or HIV, are more susceptible to developing pleural empyema.
Symptoms of Pleural Empyema
The symptoms of pleural empyema can vary depending on the severity of the infection and the individual’s overall health. Some of the most common signs and symptoms include:
- Chest Pain: Patients often experience sharp or stabbing pain in the chest, which may worsen with deep breaths or coughing.
- Fever and Chills: A high fever, often accompanied by chills, is a typical sign of infection.
- Shortness of Breath: As the pleural space fills with pus, it can compress the lungs, making it difficult to breathe.
- Cough: A persistent cough, sometimes producing foul-smelling sputum, may develop.
- Fatigue: Generalized weakness and fatigue are common in individuals with pleural empyema.
- Rapid Heart Rate: An increased heart rate may occur as the body tries to compensate for reduced oxygen levels.
Diagnosis of Pleural Empyema
Diagnosing pleural empyema involves a combination of clinical evaluation, imaging studies, and laboratory tests. Early and accurate diagnosis is crucial for effective treatment. Below are the key steps involved in diagnosing this condition:
Physical Examination
A healthcare provider will begin by conducting a thorough physical examination. They will listen to the patient’s breathing using a stethoscope to detect abnormal sounds, such as decreased breath sounds or crackles. The presence of chest pain and other symptoms will also be assessed.
Imaging Studies
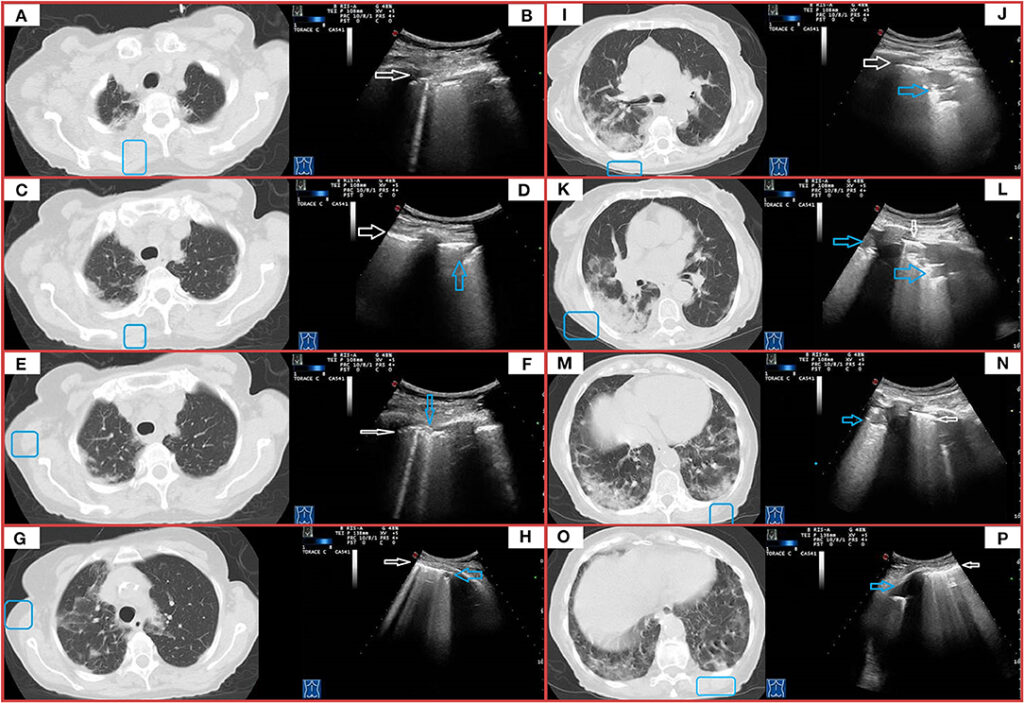
Imaging tests play a critical role in confirming the presence of pleural empyema. These include:
- Chest X-Ray: A chest X-ray can reveal fluid accumulation in the pleural space, often appearing as a shadow or opacity.
- Computed Tomography (CT) Scan: A CT scan provides a more detailed view of the chest and can help identify the extent of the infection and any underlying causes.
- Ultrasound: Ultrasound imaging is useful for guiding procedures such as thoracentesis, where fluid is removed from the pleural space for analysis.
Laboratory Tests
Fluid obtained from the pleural space through thoracentesis is analyzed in the laboratory to confirm the presence of infection. Key tests include:
- Gram Stain and Culture: These tests identify the specific bacteria causing the infection, which helps guide antibiotic therapy.
- White Blood Cell Count: An elevated white blood cell count in the pleural fluid indicates an active infection.
- pH and Glucose Levels: Low pH and glucose levels in the pleural fluid are characteristic of empyema.
Treatment of Pleural Empyema
The treatment of pleural empyema typically involves a combination of antibiotics, drainage of the infected fluid, and, in some cases, surgery. The goal of treatment is to eliminate the infection, prevent complications, and restore normal lung function.
Antibiotic Therapy
Antibiotics are the cornerstone of treatment for pleural empyema. Initially, broad-spectrum antibiotics are administered intravenously to target a wide range of bacteria. Once the specific bacteria are identified through laboratory tests, the antibiotic regimen may be adjusted to target the causative organism more effectively. Commonly used antibiotics include:
- Penicillins: Effective against many types of bacteria, especially when combined with beta-lactamase inhibitors.
- Cephalosporins: Often used in combination with other antibiotics for severe infections.
- Clindamycin: Useful for treating anaerobic bacterial infections.
Drainage Procedures
Removing the infected fluid from the pleural space is essential for recovery. Several methods can be used to achieve this:
- Thoracentesis: A needle is inserted into the pleural space to remove fluid. This procedure is often used for diagnostic purposes and to relieve symptoms in mild cases.
- Chest Tube Insertion: A chest tube is placed into the pleural space to continuously drain the infected fluid. This method is commonly used for moderate to severe cases.
- Intrapleural Fibrinolytics: Medications such as tissue plasminogen activator may be administered through the chest tube to break down thick pus and improve drainage.
Surgical Interventions
In cases where drainage and antibiotics are insufficient, surgery may be required. Surgical options include:
- Video-Assisted Thoracoscopic Surgery (VATS): A minimally invasive procedure where a camera and instruments are used to remove infected tissue and fluid.
- Decortication: This procedure involves removing the thick layer of pus and fibrous tissue that can form around the lungs, allowing them to expand properly.
- Open Thoracotomy: In severe or complex cases, open surgery may be necessary to thoroughly clean the pleural space.
Supportive Care
In addition to targeted treatments, supportive care is essential for managing pleural empyema. This includes:
- Oxygen Therapy: Supplemental oxygen may be provided to improve breathing and oxygen levels in the blood.
- Pain Management: Pain relievers are prescribed to alleviate chest pain and discomfort.
- Nutritional Support: Adequate nutrition is important for supporting the immune system and promoting healing.
Complications of Pleural Empyema
If left untreated, pleural empyema can lead to serious complications, including:
- Sepsis: A life-threatening condition where the infection spreads throughout the body.
- Lung Damage: Prolonged compression of the lungs by pus can result in permanent scarring and reduced lung function.
- Bronchopleural Fistula: An abnormal connection between the bronchi and the pleural space, which can complicate treatment.
Prevention of Pleural Empyema
While not all cases of pleural empyema can be prevented, certain measures can reduce the risk of developing this condition:
- Vaccination: Vaccines for pneumonia and influenza can help prevent respiratory infections that may lead to empyema.
- Timely Treatment of Infections: Prompt treatment of respiratory infections, such as pneumonia, can prevent the spread of bacteria to the pleural space.
- Proper Wound Care: After chest trauma or surgery, proper wound care is essential to minimize the risk of infection.