Placenta previa, often abbreviated as PP, is a condition that occurs during pregnancy when the placenta partially or completely covers the opening of the cervix. This can lead to severe bleeding before or during delivery, posing risks to both the mother and the baby. Understanding this condition, its causes, symptoms, diagnosis, and treatment options is crucial for ensuring safe outcomes for pregnant individuals. In this article, we will explore all aspects of this condition in detail.

What Is Placenta Previa?
Placenta previa is a medical condition that affects some pregnancies, particularly in the third trimester. The placenta is an organ that develops in the uterus during pregnancy and provides oxygen and nutrients to the growing baby while removing waste products. Normally, the placenta attaches to the upper part of the uterus, away from the cervix. However, in cases of placenta previa, the placenta attaches near or over the cervical opening, which can cause complications.
There are three main types of placenta previa:
- Complete placenta previa: The placenta entirely covers the cervical opening.
- Partial placenta previa: The placenta partially covers the cervical opening.
- Marginal placenta previa: The edge of the placenta lies close to the cervical opening but does not cover it.
Causes of Placenta Previa
The exact cause of placenta previa is not always clear, but several factors are believed to contribute to its development. These include:
Previous Cesarean Deliveries
Women who have had one or more cesarean deliveries are at a higher risk of developing placenta previa. Scarring in the uterine lining from previous surgeries can affect how the placenta attaches during subsequent pregnancies.
Multiple Pregnancies
Pregnancies involving twins, triplets, or more increase the likelihood of placenta previa. The larger size of the placenta required to support multiple babies may make it more likely to cover the cervical opening.
Advanced Maternal Age
Pregnant individuals over the age of thirty-five are at a higher risk of developing this condition. Age-related changes in the uterine lining may play a role in abnormal placental attachment.
Smoking During Pregnancy
Smoking has been linked to an increased risk of placenta previa. The chemicals in cigarettes may affect blood flow to the uterus, influencing where the placenta implants.
Prior Uterine Surgeries or Procedures
Surgeries such as dilation and curettage or other procedures that involve the uterine lining can leave scar tissue, increasing the chances of placenta previa in future pregnancies.
Symptoms of Placenta Previa
Placenta previa often presents with specific symptoms, particularly during the second and third trimesters. Recognizing these signs early can help ensure timely medical intervention. Common symptoms include:
Bright Red Vaginal Bleeding
One of the hallmark symptoms of placenta previa is painless, bright red vaginal bleeding. This typically occurs after the twentieth week of pregnancy and may happen suddenly without warning. The bleeding can range from mild to severe and may stop and start intermittently.
Painless Bleeding
Unlike other causes of bleeding during pregnancy, such as placental abruption, placenta previa usually does not cause pain. This characteristic makes it easier for healthcare providers to differentiate between conditions.
Uterine Contractions
In some cases, individuals with placenta previa may experience contractions along with bleeding. While contractions are common during pregnancy, their presence alongside bleeding should prompt immediate medical attention.
Abnormal Position of the Baby
Due to the position of the placenta, the baby may be in a breech or transverse position rather than the typical head-down position. This can sometimes be detected during routine ultrasounds.
Diagnosis of Placenta Previa
Early and accurate diagnosis of placenta previa is essential to manage the condition effectively and prevent complications. Healthcare providers use several methods to diagnose this condition:
Routine Ultrasound
An ultrasound is the primary tool used to diagnose placenta previa. During routine prenatal visits, healthcare providers perform ultrasounds to assess fetal growth and development. If the placenta is found to be covering or near the cervical opening, further evaluation is conducted.
Transvaginal Ultrasound
In some cases, a transvaginal ultrasound may be necessary for a clearer view of the placenta’s position. This type of ultrasound involves inserting a probe into the vagina and provides more detailed images compared to abdominal ultrasounds.
Magnetic Resonance Imaging
While less commonly used, magnetic resonance imaging may be employed in complex cases to obtain highly detailed images of the placenta and surrounding structures.
Treatment Options for Placenta Previa
Treatment for placenta previa depends on various factors, including the severity of the condition, the gestational age of the baby, and the overall health of the pregnant individual. Management strategies aim to minimize risks to both the mother and the baby.
Monitoring and Observation
For cases diagnosed early in pregnancy, especially before the twenty-eighth week, healthcare providers may recommend close monitoring. Many times, the placenta moves away from the cervical opening as the uterus expands. Regular ultrasounds are performed to track the placenta’s position.
Activity Restrictions
To reduce the risk of bleeding, individuals with placenta previa may be advised to avoid strenuous activities, sexual intercourse, and heavy lifting. Bed rest may also be recommended in certain cases to minimize pressure on the placenta.
Hospitalization
If significant bleeding occurs, hospitalization may be necessary to monitor the pregnant individual and provide immediate care if needed. Intravenous fluids and blood transfusions may be administered to address blood loss.
Medications
In cases where preterm delivery is a concern, medications may be given to delay labor and promote fetal lung maturity. Corticosteroids are commonly used to accelerate lung development in the baby if early delivery becomes necessary.
Cesarean Delivery
Most cases of placenta previa require delivery via cesarean section to avoid the risks associated with vaginal delivery. The timing of the surgery depends on the stability of the pregnant individual and the baby’s readiness for birth. In some cases, delivery may be scheduled as early as thirty-six weeks if the condition poses significant risks.
Emergency Care
In situations where severe bleeding occurs, emergency medical intervention is critical. Immediate steps are taken to stabilize the pregnant individual, and an emergency cesarean delivery may be performed to protect the lives of both the mother and the baby.
Lifestyle Adjustments and Support
Living with placenta previa can be challenging, but certain lifestyle adjustments and support systems can help individuals manage the condition effectively:
Emotional Support
A diagnosis of placenta previa can be stressful and anxiety-inducing. Seeking emotional support from loved ones, support groups, or mental health professionals can help individuals cope with the emotional toll of the condition.
Nutritional Guidance
Maintaining a healthy diet rich in iron and other essential nutrients is important to combat potential anemia caused by bleeding episodes. Consulting with a nutritionist can provide personalized dietary recommendations.
Education and Awareness
Understanding the condition and being aware of potential complications empowers individuals to make informed decisions about their care. Attending prenatal classes and staying informed through reliable sources can be beneficial.
Complications Associated with Placenta Previa
While placenta previa can be managed effectively with proper care, it is associated with certain risks and complications:
Severe Bleeding
Excessive bleeding before or during delivery is one of the most significant risks. This can lead to maternal anemia, shock, or even life-threatening situations if not promptly addressed.
Preterm Birth
Placenta previa increases the likelihood of preterm delivery, which can result in complications for the baby, such as respiratory distress syndrome or developmental delays.
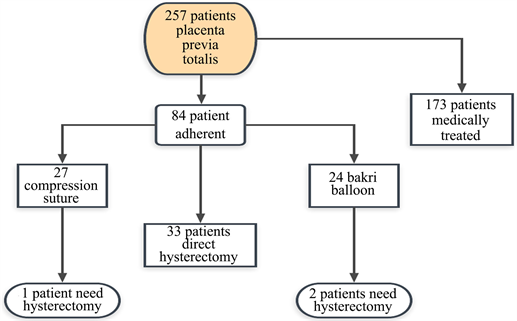
Placenta Accreta
In some cases, placenta previa is associated with placenta accreta, a condition where the placenta grows too deeply into the uterine wall. This can complicate delivery and may require a hysterectomy to remove the uterus.
Growth Restriction
Babies born to mothers with placenta previa may experience intrauterine growth restriction due to reduced blood flow through the placenta.