Placenta accreta spectrum (PAS) is a serious pregnancy-related condition that occurs when the placenta attaches too deeply into the uterine wall. This abnormal attachment can lead to severe complications during childbirth, making it a significant concern for both healthcare providers and expectant mothers. Understanding the causes, risks, diagnostic methods, and treatment options for this condition is essential for ensuring better outcomes for affected women and their babies.
Understanding Placenta Accreta
Placenta accreta is a medical condition where the placenta grows too deeply into the lining of the uterus. In normal pregnancies, the placenta detaches from the uterine wall after delivery. However, in cases of placenta accreta, the placenta remains attached, leading to potentially life-threatening bleeding. There are three main types of this condition:
- Placenta accreta: The placenta attaches too deeply but does not penetrate the uterine muscle.
- Placenta increta: The placenta penetrates into the uterine muscle.
- Placenta percreta: The placenta grows through the uterine wall and may invade nearby organs, such as the bladder.
Causes of Placenta Accreta
The exact cause of placenta accreta is not fully understood, but several factors increase the risk of developing this condition. These include:
Prior Cesarean Deliveries
Women who have had one or more cesarean deliveries are at a higher risk of developing placenta accreta. The scar tissue from previous surgeries can disrupt the normal structure of the uterine wall, making it easier for the placenta to attach too deeply.
Previous Uterine Surgeries
In addition to cesarean sections, other uterine surgeries, such as fibroid removal or dilation and curettage, can also increase the likelihood of placenta accreta. Any procedure that alters the uterine lining can create an environment conducive to abnormal placental attachment.
Advanced Maternal Age
Women over the age of 35 are more likely to experience placenta accreta. As maternal age increases, so does the risk of complications during pregnancy, including abnormal placental attachment.
Placenta Previa
Placenta previa, a condition where the placenta partially or completely covers the cervix, is strongly associated with placenta accreta. Women diagnosed with placenta previa are often closely monitored for signs of placenta accreta due to the increased risk.
Multiparity
Having multiple pregnancies, especially if they involve cesarean deliveries, can elevate the risk of placenta accreta. Each pregnancy adds to the cumulative effect of scarring and changes in the uterine wall.
Risks Associated with Placenta Accreta
Placenta accreta poses significant risks to both the mother and the baby. These risks include:
Severe Hemorrhage
One of the most immediate and dangerous complications of placenta accreta is severe bleeding during or after delivery. When the placenta fails to detach properly, attempts to remove it can result in uncontrollable hemorrhage, which may require emergency intervention.
Hysterectomy
In many cases, the only way to stop the bleeding caused by placenta accreta is through a hysterectomy, or the surgical removal of the uterus. While this procedure can save the mother’s life, it also means she will no longer be able to bear children.
Premature Birth
Placenta accreta often necessitates early delivery to minimize risks to the mother. Babies born prematurely may face a range of health challenges, including respiratory difficulties, developmental delays, and low birth weight.
Damage to Nearby Organs
In cases of placenta percreta, the placenta can invade nearby organs, such as the bladder or intestines. This invasion can lead to additional complications, including organ damage and infection.
Diagnosis of Placenta Accreta
Early diagnosis of placenta accreta is crucial for planning appropriate care and minimizing risks. Several diagnostic tools and techniques are used to identify this condition:
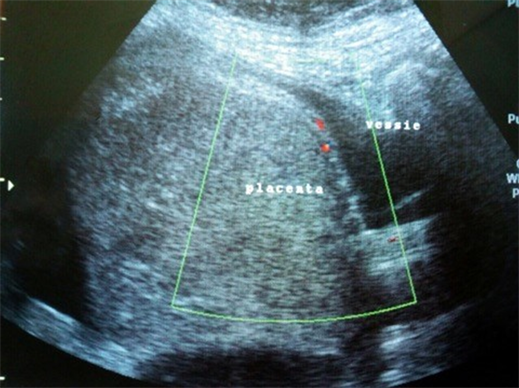
Ultrasound Imaging
Ultrasound is the primary tool used to diagnose placenta accreta. A transabdominal or transvaginal ultrasound can reveal abnormalities in the placental attachment, such as loss of the clear zone between the placenta and the uterine wall.
Magnetic Resonance Imaging
In cases where ultrasound results are inconclusive, magnetic resonance imaging may be used to provide a more detailed view of the placenta and surrounding structures. MRI can help determine the depth of placental invasion and assess potential involvement of nearby organs.
Clinical Evaluation
A thorough clinical evaluation, including a review of the patient’s medical history and risk factors, is essential for diagnosing placenta accreta. Healthcare providers will consider factors such as prior cesarean deliveries, placenta previa, and uterine surgeries when assessing the likelihood of this condition.
Treatment Options for Placenta Accreta
The management of placenta accreta depends on the severity of the condition, the gestational age of the fetus, and the overall health of the mother. Treatment options include:
Planned Cesarean Hysterectomy
For women with confirmed placenta accreta, a planned cesarean hysterectomy is often recommended. This procedure involves delivering the baby via cesarean section followed immediately by the removal of the uterus. Planning this surgery in advance allows healthcare providers to prepare for potential complications and ensure the availability of blood transfusions and other resources.
Conservative Management
In some cases, conservative management may be considered, particularly for women who wish to preserve their fertility. This approach involves leaving the placenta in place after delivery and allowing it to dissolve naturally over time. However, this option carries a higher risk of infection and delayed hemorrhage, requiring close monitoring and follow-up care.
Uterine Artery Embolization
Uterine artery embolization is a minimally invasive procedure that can be used to reduce blood flow to the placenta and control bleeding. This technique may be employed as part of a broader treatment plan to manage placenta accreta and minimize the need for extensive surgery.
Preterm Delivery
In cases where placenta accreta poses a significant risk to the mother, preterm delivery may be necessary. Balancing the risks to the mother with the developmental needs of the baby is a critical consideration in these situations.
Supportive Care and Multidisciplinary Approach
Managing placenta accreta requires a multidisciplinary team of healthcare professionals, including obstetricians, maternal-fetal medicine specialists, radiologists, anesthesiologists, and surgeons. This collaborative approach ensures comprehensive care and improves outcomes for both the mother and the baby.
Supportive care measures, such as regular monitoring, nutritional support, and psychological counseling, are also important components of managing placenta accreta. Women diagnosed with this condition may experience anxiety and stress, and addressing their emotional well-being is essential for overall health.
Emerging Research and Advances
Ongoing research is focused on improving the understanding, diagnosis, and treatment of placenta accreta. Advances in imaging technology, surgical techniques, and postpartum care are helping to enhance outcomes for affected women. Additionally, studies exploring the genetic and molecular factors underlying placenta accreta may lead to new preventive strategies in the future.





